Blood test could help doctors monitor effectiveness of hay fever immunotherapy
by Sam Wong

A new test for measuring histamine release from certain white blood cells could help doctors monitor the effectiveness of immunotherapy for hay fever.
Immunotherapy involves exposing patients to gradually increasing doses of allergen by injection or through tablets or drops placed under the tongue to ‘desensitise’ their immune systems. It is widely used for people with severe allergies who don’t respond to drug treatment. But better methods are needed to identify who will respond best to this treatment and monitor its effect.
Allergic reactions are triggered when two types of white blood cells, mast cells and basophils, release histamine, a signalling chemical that promotes symptoms like itching, swelling and sneezing. Immunotherapy works in part by reducing histamine release from basophils, but histamine itself is difficult to measure accurately.
Researchers at Imperial College London have shown that the enzyme diamine oxidase (DAO) can be used to measure histamine release from basophils. This will allow doctors to monitor how responsive basophils are to allergens such as grass pollen in the test tube, and in doing so may give an indication of the effectiveness of the treatment.
The study was led by Dr Mohamed Shamji and Professor Stephen Durham at the National Heart and Lung Institute at Imperial, and published in the Journal of Allergy and Clinical Immunology.
“Immunotherapy works very well for most patients with severe hay fever, but a proportion of them don’t respond,” said Professor Durham. “Having the therapy is a big commitment – you have to attend clinic on multiple occasions, and currently there are no markers to assess how well it’s working. This novel test developed by Dr Shamji for grass allergic patients could easily be translated to hospital immunology labs, and so has the potential to be used in clinical practice.”
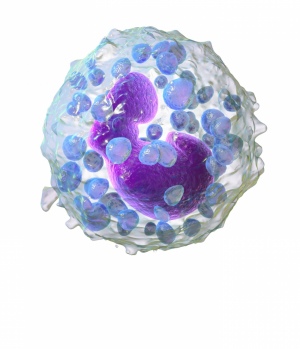
3D rendering of a basophil containing histamine granules. By Blausen.com staff.
The team took small blood samples from volunteers with hay fever, some of whom were undergoing immunotherapy at Royal Brompton Hospital, and non-allergic volunteers without hayfever. They then used the new method to measure the basophils’ response to grass pollen.
DAO binds to histamine, allowing scientists to measure histamine in basophils by labelling DAO with a fluorescent marker that can be detected with lab equipment.
When the researchers added grass pollen to the blood of non-allergic volunteers in the lab, the basophils did not release histamine, whereas significant histamine release was measured from the cells of allergic volunteers. In volunteers undergoing immunotherapy, less histamine was released and the amount correlated with the severity of their hay fever symptoms.
“A great advantage of allergen immunotherapy is that it induces long-term benefits and it is likely that the diamine oxidase test will allow monitoring of disease activity in individuals after discontinuation of the treatment,” said Professor Durham.
In another study published recently in the same journal, the Imperial team identified a role for a new subset of immune cells in hay fever. Numbers of these cells, called innate lymphoid type 2 cells (ILC2s), increased in the blood of hay fever sufferers during the pollen season. This increase was inhibited in patients undergoing immunotherapy, suggesting immunotherapy may work in part by controlling the number of ILC2s.
“These findings provide further insight into how the disease works and ILC2s could also be a target for development of new therapies,” said Dr Shamji.
Both studies were funded by the Immune Tolerance Network.
References
M.H. Shamji et al. ‘Basophil expression of diamine oxidase: A novel biomarker of allergen immunotherapy response.’ Journal of Allergy and Clinical Immunology, 2014. http://dx.doi.org/10.1016/j.jaci.2014.09.049
M. Lao-Araya et al. ‘Seasonal increases in peripheral innatelymphoid type 2 cells are inhibited by subcutaneous grass pollen immunotherapy.’ Journal of Allergy and Clinical Immunology, 2014. DOI: http://dx.doi.org/10.1016/j.jaci.2014.07.029
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Sam Wong
School of Professional Development