The quest for an HIV vaccine
How the international project EAVI2020 has boosted HIV vaccine research
HIV: a global problem
Since COVID-19 reared its head in December 2019, the global scientific community has developed several effective vaccines against the virus. The US Food and Drug Administration (FDA) approved the Pfizer-BioNTech vaccine in December 2020, just one year after COVID-19 was first detected.
HIV has been around for decades. The number of people living with HIV continues to rise and hundreds of thousands of people around the world die every year from the disease, yet no effective vaccine exists.
“We’ve been trying to develop a vaccine for HIV for over 30 years as a field,” says Professor Robin Shattock, Head of Mucosal Infection and Immunity within the Faculty of Medicine at Imperial College London.
“It still remains one of the biggest biological challenges of a generation.”

Introducing EAVI2020
International problems require international solutions.
If the past few years have taught us anything, it’s that science is at its best when researchers come together to work towards a common goal.
This was the basis of the European AIDS Vaccine Initiative (EAVI2020). Launched in 2015, and concluding in December 2022, EAVI2020 was a 23 million euro project funded by the European Commission. The project brought together 22 teams with different expertise and ideas from across Europe, with additional partners in Australia and Canada, to further progress towards an HIV vaccine.
“There was a great sense of excitement,” recalls Professor Shattock, who led the project. “We were bringing together teams from all across Europe at a critical time in HIV research where scientific progress had revealed unprecedented insight into the nature of protective antibodies and anti-viral cellular responses that are needed for an effective vaccine.”
The EAVI2020 consortium members consisted of molecular biologists, immunologists, virologists, biotechnologists and clinicians. Collectively, they provided the breadth of expertise required to take the latest discoveries in the lab and rapidly advance them through preclinical testing and manufacture, and into early-stage human trials.
Sites of EAVI2020's partners in Europe (left), Canada (top right), and Australia (bottom right)
Sites of EAVI2020's partners in Europe (left), Canada (top right), and Australia (bottom right)
Where to begin?
You may wonder how a project would even start to approach a problem like developing an HIV vaccine.
Firstly, we need to understand that there are two main kinds of possible HIV vaccine:
- Preventative (or prophylactic): the classic idea of a vaccine, where receiving the vaccine prevents you from contracting the infection and/or developing disease.
- Therapeutic (or curative): a vaccine that would be given to someone with an existing infection, aiming to boost the immune system so that the body can slow or eradicate the virus.
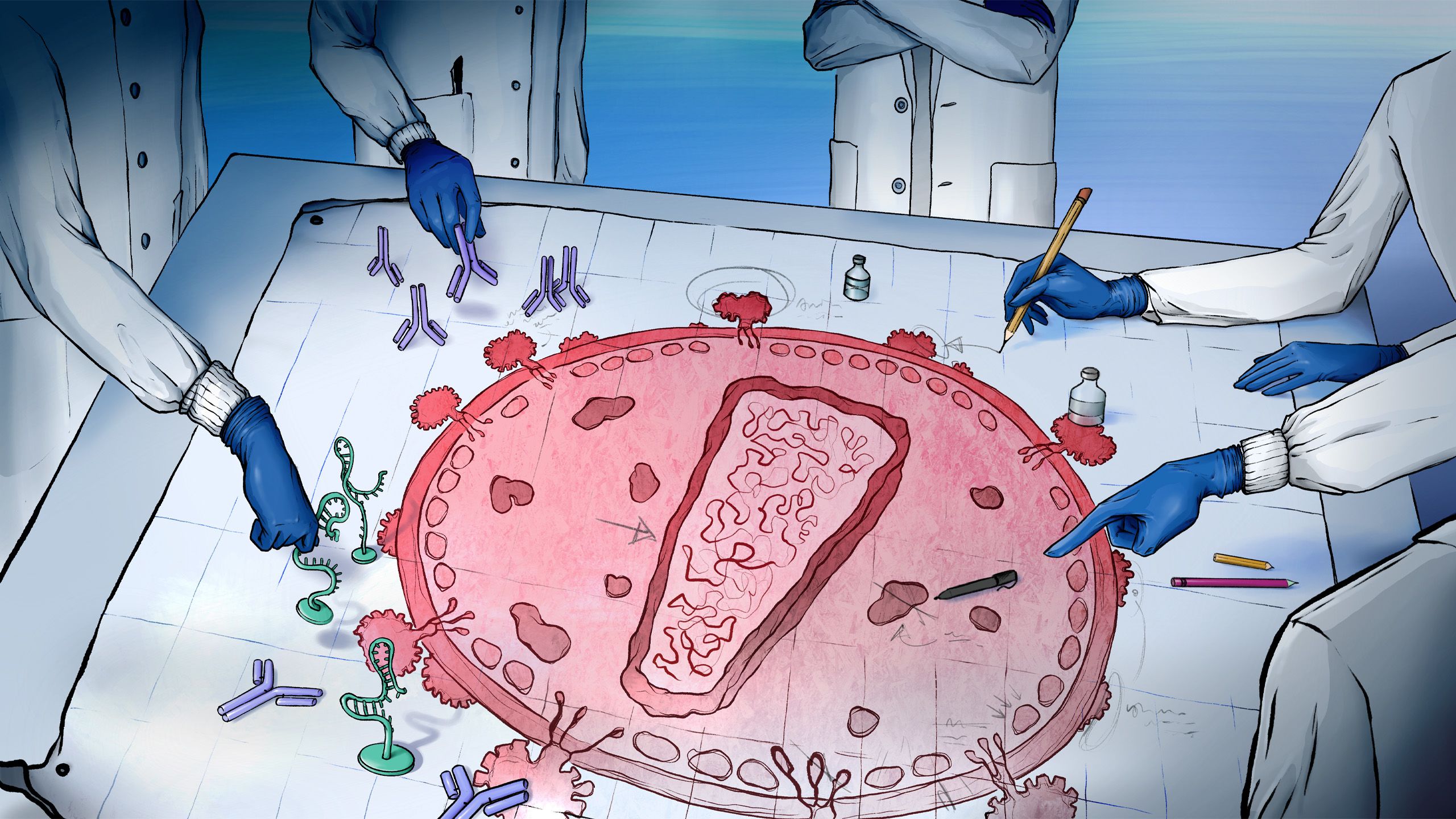
Both approaches would need to create a strong immune response in order to fight off HIV. There are two arms of the body’s immune system that a vaccine can focus on inducing – ‘humoral’ and ‘cellular’.
The humoral immune response relies on the vaccine activating B cells, a type of immune cell, to produce antibodies that bind to the virus and prevent it from infecting your cells.
The cellular immune response is where T cells, another type of immune cell, seek out and kill infected cells.
“Tackling both of those approaches was important because in our minds we knew we'd have to bring together both arms of the adaptive immune responses to develop an effective vaccine,” says Professor Shattock.
Knowing this is all well and good, but actually inducing these immune responses against HIV is where things get tricky.

Chasing a moving target
Viruses are known to mutate – everyone will recall that there have been several well-documented variants of COVID-19. But HIV operates on another scale, mutating incredibly quickly to produce new strains.
Not only are there many, many strains of HIV globally, but the virus is also variable even within a single infected individual.
“The variability of viral strains of SARS-CoV-2 is probably much lower than that of HIV within a single infected individual,” explains Professor Shattock. “So, the problem is orders of magnitude greater for HIV. There’s just so many strains, and the virus can change so quickly, that being able to have a vaccine that can keep up with that moving target is proving particularly challenging.”
The continuously changing nature of HIV means that the body’s immune system finds it very difficult to produce antibodies that can fight off the virus, as it can rapidly change itself so that those antibodies are no longer effective.
Professor Rogier Sanders from Universitair Medische Centra in Amsterdam led EAVI2020’s charge in developing approaches to stimulate the production of effective antibodies against HIV, bringing with him the results of his previous research.
“I had been working on HIV envelope vaccines for a long time,” says Professor Sanders. “We had somewhat of a breakthrough just before EAVI2020 started with the development of what we call ‘native-like envelope trimers’. The envelope protein is on the outside of the virus, but it’s unstable and falls apart easily when you try to put it into a vaccine. My team managed to stabilise it in such a way that it can be expressed in a vaccine candidate without worrying that it’ll fall apart.”
Professor Rogier Sanders, Universitair Medische Centra, Amsterdam
Professor Rogier Sanders, Universitair Medische Centra, Amsterdam
Professor Sanders and his team took around 20 years to develop just one example of this kind of vaccine, but managed to create eight new versions of this design and entering them in clinical studies over the course of EAVI2020. These were some of the first clinical trials to be looking at this kind of vaccine.
Whilst Professor Sanders focussed his efforts on developing a vaccine to induce the humoral arm of the immune system, Professors Tomáš Hanke from the University of Oxford and Christian Brander from IrsiCaixa, Barcelona, took on the challenge of inducing the body’s cellular immune protection.
Professor Tomáš Hanke and his team at the University of Oxford. Left to right: Yehia Mohamed, Edmund (Edd) Wee, Nathifa Moyo, Nicola Borthwick, Zara Hannoun and Tomáš Hanke.
Professor Tomáš Hanke and his team at the University of Oxford. Left to right: Yehia Mohamed, Edmund (Edd) Wee, Nathifa Moyo, Nicola Borthwick, Zara Hannoun and Tomáš Hanke.
“The main challenge is the same – the variability of the virus,” says Professor Hanke. “But the problems associated with tackling this variability is different between inducing broadly neutralising antibodies and inducing protective killer T cells.”
The vaccine candidate designed by Professor Hanke tackles this variability by focusing on the most conserved parts of the HIV virus, which are the parts that change the least and are common to most global variants as well.
Professor Brander notes that a possible solution comes from some people living with HIV themselves.
“We know that there are some people with good control of the virus on their own without having to take antiretrovirals. Everyone who becomes infected with the virus makes a roaring T cell response, which is, however, mostly inefficient. In a previous study, we found specific regions of HIV, responses to which were associated with low virus load, so we combined them into a singular construct to test in a vaccine.”
Professor Christian Brander, IrsiCaixa, Barcelona
Professor Christian Brander, IrsiCaixa, Barcelona
Test and analysis
Developing vaccine candidates is just one step towards an effective HIV vaccine. Each of these candidates must go through rigorous testing and analysis for both safety and effectiveness.
Candidate vaccines had to leap various hurdles as part of the EAVI2020 project, being tested first in rabbits, then macaques (a type of monkey), before being trialled in humans.
Dr Nathalie Dereuddre-Bosquet, Commissariat à l’Energie Atomique et aux Energies Alternatives (CEA), Paris
Dr Nathalie Dereuddre-Bosquet, Commissariat à l’Energie Atomique et aux Energies Alternatives (CEA), Paris
“A key part of EAVI2020 involved finding which animal models are the most predictive [of results in humans], in order to reduce the number of animals that have to be tested on in future projects,” says Dr Nathalie Dereuddre-Bosquet, a specialist in non-human primate immunology and on preclinical models for vaccine development from the Infectious Disease Models and Innovative Therapies (IDMIT) Infrastructure within the Commissariat à l’Energie Atomique et aux Energies Alternatives (CEA) in Paris.
“We only use macaques in late-stage preclinical development of vaccines for the most promising candidates. It’s important to test vaccines in macaques as their immune systems and physiology are really much closer to humans. For instance, non-human-primate models are crucial to identify and understand interactions between B-cell and T-cell vaccines.”
Only vaccines that overcome these hurdles can then be trialled in humans, initially in a small group to measure safety, before going onto larger groups to test how well the vaccine actually works.
A key player involved at all stages of this process is Dr Gabriella Scarlatti from Ospedale San Raffaele in Milan, whose team analyses biological material, such as blood samples, to ascertain whether the vaccine is good enough to progress.
Dr Gabriella Scarlatti, Ospedele San Rafaelle, Milan
Dr Gabriella Scarlatti, Ospedele San Rafaelle, Milan
“We had the task of testing the samples to see if there is a change between before and after immunisation,” says Dr Scarlatti. “For example, we want to see if vaccines have increased capacity to induce neutralising antibodies. Neutralizing antibodies are the Holy Grail of HIV vaccinology as they not only bind to the virus but also prevent it from entering and infecting the cell.”
Another aspect that Dr Scarlatti’s team looked for were broadly reactive antibodies i.e. antibodies that could neutralise multiple strains of HIV. This is vital so that any future vaccine can deliver as much protection as possible.
A two-pronged approach
EAVI2020 ran eight clinical studies in humans during the course of its project, most of which have finished, but some are still underway at the time of writing.
A key trial for Professor Brander is one that is understatedly named BCN03. This is testing a vaccine that brings together his work on inducing the cellular immune response with Professor Sanders’ work on inducing broadly neutralizing antibodies.
“BCN03 is the first therapeutic vaccine trial that combines T and B cell immunogens,” says Professor Brander. “In EAVI2020, we always wanted to produce B cell and T cell immunogens and to test them individually, but we managed to combine them together, which was originally planned to be achieved after the project.”
Currently, in the therapeutic setting, the focus is on inducing the cellular immune responses – teaching T cells to kill cells producing HIV. They’re now layering in inducing humoral immunity as well.
This concept is new, and in Professor Brander’s opinion, very promising.
“For me this is really one of the culminations of the programme, especially because it’s ahead of what we planned to achieve during EAVI2020.
“Getting a better appreciation for the importance of having the humoral immune response and the cellular immune response coming together, and studying their interactions, is vital for both the therapeutic and the preventative setting.”
COVID-19: disruption and innovation
An unexpected spanner in the works came in the form of the COVID-19 pandemic.
“When the COVID-19 pandemic took off, there were many restrictions across Europe and the EAVI2020 sites,” says Professor Shattock. “Many EAVI2020 laboratories closed or were repurposed for COVID-19 projects, affecting our HIV projects and clinical programmes.
“Many of the consortium members also contributed either on the frontlines or into vaccine development for COVID-19.”
Professor Shattock himself led Imperial College London’s COVID-19 vaccine development programme and played a large role in the public awareness and understanding of vaccines in the UK.
Despite the impact of the pandemic on both the project and the world as a whole, there was a silver lining to the dark COVID cloud: the fantastic success of mRNA-based vaccines, which includes the Pfizer-BioNTech vaccine.
mRNA vaccines use a molecule called messenger RNA, which the body creates when expressing genes and acts as a blueprint for a protein molecule. mRNA vaccines use a piece of mRNA that corresponds to a protein from the virus it’s looking to target. The body’s cells then make the protein, which the immune system can react to and then remember if the body gets infected with the real virus.
Many of the vaccines that EAVI2020 had been developing up to this point were more complex and expensive to make compared to mRNA vaccines. BioNTech were one of the EAVI2020 partners looking at mRNA vaccines for HIV.
As the project managed to get up and going again, the team invested more effort into mRNA approaches for HIV as it meant they could create and test more vaccine candidates more quickly.
“We managed to design and make brand new HIV vaccine candidates and tested them in the clinic in a matter of five years, which is really incredible, especially for the protein vaccines. Now with RNA, things will accelerate even further,” says Professor Sanders.
More of the mRNA-based candidates have now been moved into pre-clinical studies, which Professor Shattock notes is already producing promising data that could be important for HIV vaccine development moving beyond EAVI2020 as the project comes to an end.

A success of collaboration
“The greatest achievement [of EAVI2020] has been the success in bringing a large number of new vaccine candidates into clinical trials,” says Professor Shattock. “For people who don’t inhabit this space, we have managed to produce more vaccines, test more vaccines, than any other programme of a similar scale, or even some funded to a much larger extent.
“But another thing I’m personally very proud about is that it’s built a very effective and collaborative scientific community, not only of senior researchers but also mentored a large cohort of young investigators. And, of course, that is essential to the excellent science across Europe and in vaccine discovery.
“The success of EAVI2020 has been absolutely dependent on bringing together these multiple centres across Europe, because they all come with different expertise and with different ideas, different disciplines, and it’s that cross-interaction of different teams that is really synergistic.
“So, what’s been achieved could not have been achieved if all those groups had been funded individually, independently. It’s really dependent on that critical mass and being able to work together in a coordinated programme.”
“No one could have done this project on their own, because there are so many different kinds of expertise involved and everyone did their bit,” agreed Professor Sanders.
Looking to the future
“It’s been an enormous privilege to work with such a dedicated and talented team. We’re challenged by the future, but challenge drives innovation. We’re well set to build on the legacy of what’s been achieved by EAVI2020.”
Over the seven years of the project, EAVI2020 managed to develop vaccine candidates to stimulate both the humoral and cellular immune responses and was able to run many animal and human trials to test their safety and effectiveness in both preventative and therapeutic settings.
“The impressive work of EAVI2020, the continuous development and improvement of vaccine candidates, means there is an enormous amount of data and material produced in the studies that can be analysed further,” says Dr Scarlatti.
Several of the animal and human trials initiated by EAVI2020 are still ongoing, with one now being launched as the project comes to a close that will be run by Dr Scarlatti in Milan to test a new therapeutic T cell vaccine candidate designed by Professor Hanke.
The many data produced by EAVI2020, and the data still to come, are vital to making progress towards an effective HIV vaccine.
“We’re already looking for the legacy of EAVI2020,” says Professor Shattock. “We are collaborating with other groups to share some of these very sophisticated vaccines that we’ve developed that can be used in combination with approaches developed in other parts of the world. We are looking to see if any of these candidates merit additional development in their own right, or whether we should be looking at combinations.”
However, the next big challenge is finding the funding for this work.
“The HIV vaccine field is beginning to struggle for recognition and further funding because of a false feeling that HIV has been solved by antiretroviral treatment,” says Professor Hanke. “Treatment has been transformative, but it only buys time for the development of an effective vaccine, which will likely be a key part of any package to truly end the HIV epidemic.”
Whilst the future can never be certain, everyone who has contributed to EAVI2020 can be proud of the work they have done to progress the global effort to eradicate HIV, and they have shown the power of collaboration in making these strides.
“It’s been an enormous privilege to work with such a dedicated and talented team,” says Professor Shattock. “We’re challenged by the future, but challenge drives innovation. We’re well set to build on the legacy of what’s been achieved by EAVI2020.”
EAVI2020's kick-off meeting in 2015.
EAVI2020's kick-off meeting in 2015.
The EAVI2020 team at their 2016 Annual Meeting.
The EAVI2020 team at their 2016 Annual Meeting.
Due to the COVID-19 pandemic, online collaboration was key to the project. EAVI2020's 2020 Annual Meeting was held online.
Due to the COVID-19 pandemic, online collaboration was key to the project. EAVI2020's 2020 Annual Meeting was held online.
Professor Shattock and members of his team discussing HIV vaccines at the Science Museum London's Pride Lates in June 2022.
Professor Shattock and members of his team discussing HIV vaccines at the Science Museum London's Pride Lates in June 2022.
The EAVI2020 team at their penultimate meeting in the spring of 2022.
The EAVI2020 team at their penultimate meeting in the spring of 2022.

EAVI2020 Partners
EAVI2020 received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No. 681137. The sole responsibility for the content of this project lies with the authors. It does not necessarily reflect the opinion of the European Union. The European Commission is not responsible for any use that may be made of the information contained therein.







































