Our impact
Find out more about how our research is making an impact on patient safety.
Our impact
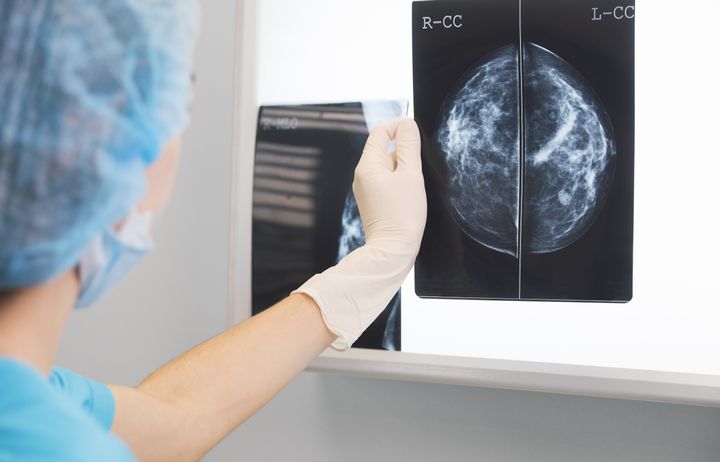
Artificial intelligence to spot breast cancer
Researchers at our Centre are part of a collaborative programme of work that is exploring whether artificial intelligence (AI) could help make breast screening more accurate, reducing the burden on clinicians and leading to better outcomes for women.
Breast screening can help save lives by spotting changes that could be cancer, enabling women to be treated earlier. In the UK, breast screening primarily takes place when women aged between 50 and 71 are invited to a mammogram every three years. The scans are reviewed by radiologists. But as human beings, mistakes can be made and some cancers may be missed, while other women may go on to receive potentially harmful treatment they didn’t need.
Working in partnership with the NIHR Imperial Biomedical Research Centre, Google Health, DeepMind, Imperial College London, the NHS and Northwestern University in the US, the research led by our director Professor Darzi designed and trained an artificial intelligence algorithm to screen mammography images from almost 29,000 women.
The AI was as good at spotting cancers as expert radiologists, highlighting the potential of AI to aid screening in the future, improving accuracy and assisting clinical staff by freeing up time and resources. The research team has now secured further funding through the Artificial Intelligence in Health and Care Award to further assess the feasibility of the system and see how the technology could be integrated into the national screening programme in the future to support clinicians.
Further work
The findings not only highlight the potential for improving accuracy and enabling technology in healthcare, but the study has also opened up new research avenues for our Centre.
In collaboration with Public Health England, one project will focus on increasing the uptake of breast screening in specific areas with low attendance, such as London, using evidence-based messaging in the screening invites.
The second project aims to use behavioural science to help understand why people choose not to attend screening. This study will engage the public to gain an awareness of common barriers to attendance. A video intervention will then be produced and tested in a trial to measure the impact on screening uptake and whether attendance can be boosted.

Data sharing to enhance patient safety
Our recent research has shown that providing people with access their own electronic health records has the potential to improve health outcomes and patient safety.
A key focus for our Centre is improving the use of data in healthcare. Building on previous research conducted by IGHI, our scientists have worked to advance understanding of the benefits and challenges of sharing medical data with patients.
By giving people who have type 2 diabetes access to their own records in electronic form, known as electronic health records (EHR), we have been able to evaluate the impact of the data sharing on care quality and health. Our findings demonstrated that letting participants see their health data helped reduce blood sugar levels, a major predictor of death, and improved safety.
The study has sparked wider conversation around data and patient safety, earning national and international recognition, including being selected as one of the British Medical Journal’s Quality & Safety’s Top Articles of 2020 and published as an NIHR Alert.
Within the research, further patient and public involvement was carried out via a web survey which assessed whether people could understand the technical nature of their health records. The study asked 1,200 people to identify potential errors in their records finding that 58.6% had no problem understanding their EHR information. This suggests that there is an opportunity to improve the presentation of information and design of the EHR, better facilitating patients’ understanding of their records and benefitting patient safety.
As the use of digital technology in healthcare increases, accelerated by the COVID-19 pandemic, this and future research will form a crucial part of the evidence base used to assess the impact of these changes on

Informing clinical decisions and reducing medication errors
Up-to-date medication prescribing data is vital for clinicians to make safe and informed decisions on the front line. Too often though, this data is fragmented and, most importantly, not machine-readable. This makes it unusable for computerised systems like clinical decision support.
Our team of clinicians have been working with engineers and designers from IGHI’s Helix Centre, in partnership with the Royal Pharmaceutical Society. Together they have developed Dosium’s Touchdose app, one of the world’s most advanced, real-time medication decision support systems to enable safe, informed decision-making.
With funding and support from research grants, including a prestigious NIHR Invention for Innovation (i4i) award, the system puts doctors, nurses and pharmacists in direct contact with the most up-to-date and patient-specific medication guidance at all times.
By integrating a range of data including patient and drug manufacturers’ information, national formularies and hospital protocols, Touchdose ensures that the right patient receives the right drug, at the right dose, at the right time. While maintaining active research engagement with IGHI, Dosium successfully spun out from Imperial College London in October 2020 and is working closely with key national authorities, leading NHS Trusts and forward-thinking technology and clinical partners to deliver detailed decision support and world-class user experiences to the clinical front line.

Learning from patient complaints
The English National Health Service receives over 200,000 complaints from patients per year. These represent an opportunity to learn from people’s experiences and drive improvement in the delivery of care, while also empowering those who provide feedback over the services they’ve accessed. Yet sometimes the issues raised are missed in healthcare settings and are therefore not responded to or addressed. This is partly as it is difficult to analyse and interpret the vast amount of feedback the NHS receives daily.
In response to this, our researchers have developed a platform called Feedback First. Freely accessible online, it provides a series of tools and resources for Trusts, researchers and patient experience organisations to support complaints teams. The platform includes the Healthcare Complaints Analysis Tool (HCAT), a coding method developed by the London School of Economics and Political Science that allows organisations to standardise the way they analyse patient complaints.
The researchers behind the website hope Feedback First will allow healthcare professionals to unite, share and learn effectively from patient complaints.
Visit the platform here.


