Natural killer
A cell therapy that harnesses one of the body's rarest immune cells – the natural killer T cell – could transform the treatment of blood cancers and other diseases.
Imperial is working with Australian company Arovella Therapeutics to clinically develop a new cell therapy that could be used to treat a range of conditions, beginning with blood cancers such as leukaemia, lymphoma, and multiple myeloma.
The immunotherapy, based on research by Professor Tassos Karadimitris and his team at Imperial’s Centre for Haematology, harnesses the invariant natural killer T (iNKT) cell, a rare type of immune cell that works alongside antibodies and T cells as part of the body’s natural immune defences. The therapy will use iNKT cells that have been combined with lab-made proteins known as chimeric antigen receptors (CARs), which cause the immune cells to recognise and activate against target cells such as cancers.
The approach resembles CAR-T therapy, an advanced and still relatively new form of medicine that combines CARs with T cells and is being successfully used to treat certain blood cancers. However, the new CAR-iNKT therapy has important potential advantages – most notably that it can be produced as an off-the-shelf treatment.

Professor Tassos Karadimitris (pictured left) and team members including Dr Kanagaraju Ponnusamy (right) are researching CAR-iNKT immunotherapy for cancer. Photo: Thomas Angus
Professor Tassos Karadimitris (pictured left) and team members including Dr Kanagaraju Ponnusamy (right) are researching CAR-iNKT immunotherapy for cancer. Photo: Thomas Angus
A new approach to immunotherapy
Conventional T cells cannot be transplanted from a donor to a recipient because they would attack the recipient's cells, a condition known as graft-versus-host disease. In CAR-T therapy, T cells are therefore taken from the patient and genetically modified to produce a bespoke medicine. This makes CAR-T therapy expensive, costing upwards of £200,000 per treatment.
iNKT cells, by contrast, can be safely transplanted from one person to another. Using a new technique developed in Professor Karadimitris’s lab, the CAR-iNKT cells used in the new therapy could be mass produced at much lower cost using iNKT cells provided by healthy donors and offered to patients as an off-the-shelf treatment.
CAR-iNKT could also prove effective at treating solid tumour cancers due to iNKT cells’ superior ability to penetrate peripheral tissue such as the stomach, pancreas, and prostate.
While clinical trials will be required to establish that the therapy is safe and effective, pre-clinical data suggests that it could also prove more effective than CAR-T therapy. Because iNKT cells are part of both the adaptive and innate immune systems, iNKT cells equipped with CARs have potential to deliver a powerful dual response to blood cancers.
In experiments on mice with the blood cancer lymphoma, the long-term survival rate was 90% after CAR-iNKT treatment compared to 60% after CAR-T. Moreover, early clinical trials by a group in Houston, USA, suggest that CAR-iNKT therapy has milder side effects than those associated with CAR-T therapy, which include neurotoxicity and cytokine release syndrome.
Professor Karadimitris plans to investigate the application of CAR-iNKT to other kinds of cancer, including solid tumour cancers, which CAR-T has proved largely ineffective against. Pre-clinical data suggests that the therapy has potential for treating cancers in the brain due to iNKT cells’ ability to cross the blood-brain barrier, and that it might also prove effective at treating solid tumour cancers in other organs due to iNKT cells’ superior ability to penetrate peripheral tissue such as the stomach, pancreas, and prostate. He is beginning work to investigate the therapy’s application to viral diseases including HIV.
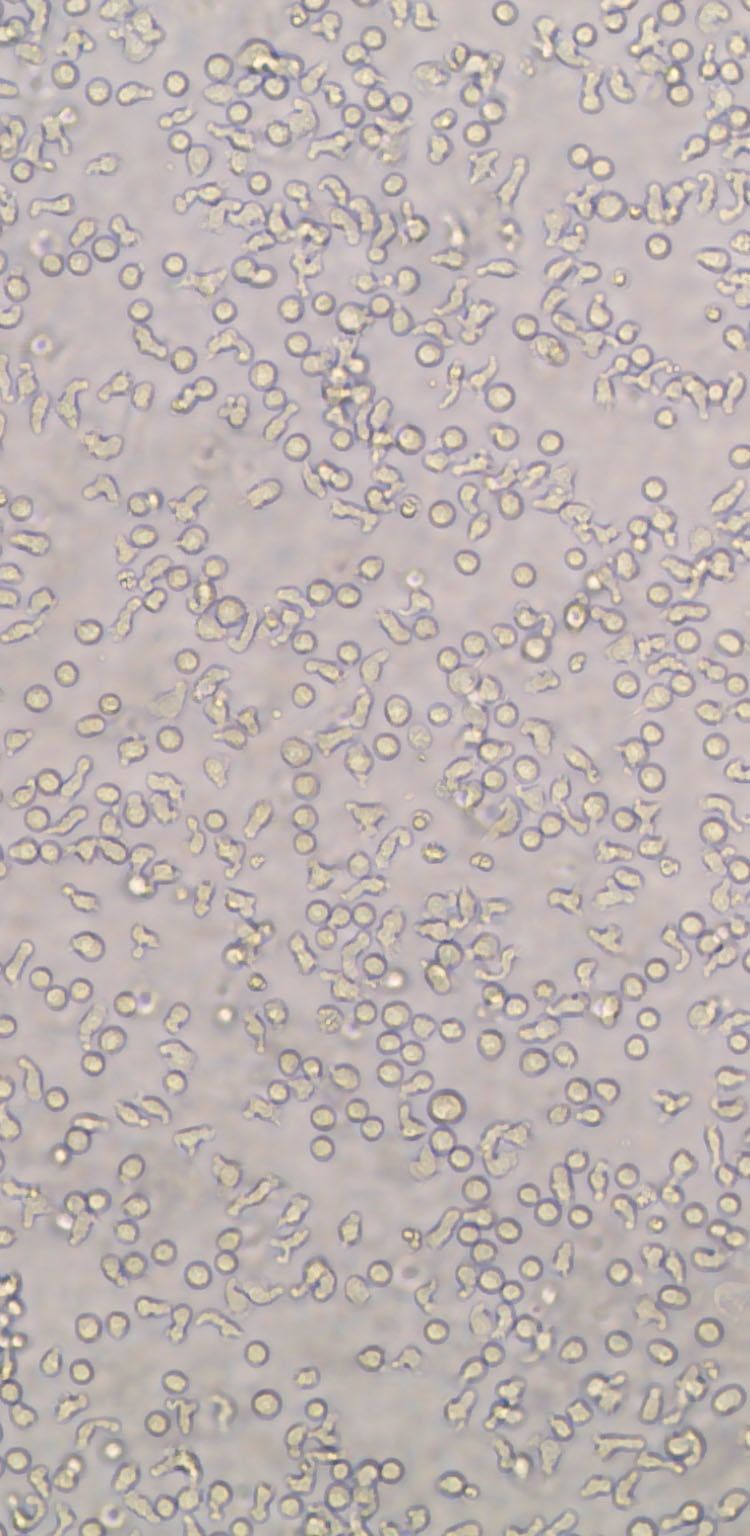
CAR-iNKT cells under the microscope as they grow
CAR-iNKT cells under the microscope as they grow
Bringing the therapy to patients
Imperial has licensed intellectual property generated by Professor Karadimitris and his team to Arovella Therapeutics, previously known as SUDA Pharmaceuticals, a biotechnology company focused on developing new medical treatments. The company will use its expertise and financial resources to progress the new therapy into clinical trials over the next one to two years, and eventually, it is hoped, deliver new treatments to patients around the world. Clinical development will focus initially on blood cancers with the possibility of expanding the approach to other cancers and other types of disease.
Cell therapies have transformed the way we think about cancer treatment. The iNKT cell therapy platform provides an opportunity to target several cancers using a product that we expect to have superior activity and to be more cost-effective.”
Imperial is working closely in partnership with the company. In addition to the licensing agreement, Professor Karadimitris and colleagues will carry out collaborative research with Arovella, and Professor Karadimitris will be the chair of Arovella's Scientific Advisory Board (SAB) for the programme.
Arovella's CEO and Managing Director, Dr Michael Baker, said: “Cell therapies have transformed the way we think about cancer treatment. The iNKT cell therapy platform provides an opportunity to target several cancers using a product that we expect to have superior activity and to be more cost-effective, which should allow the therapy to reach more individuals.”
"We are excited to solidify the partnership with Imperial College London through a research collaboration – and that Professor Karadimitris is joining us, on an independent basis, as the Chair of the SAB. We look forward to continuing the research in the laboratory of Professor Karadimitris and to broadening the platform by creating new intellectual property.”

Dr Michael Baker is the CEO and Managing Director of the Australian company Arovella Therapeutics, which is working with Imperial to bring the new cell therapy to patients.
Dr Michael Baker is the CEO and Managing Director of the Australian company Arovella Therapeutics, which is working with Imperial to bring the new cell therapy to patients.
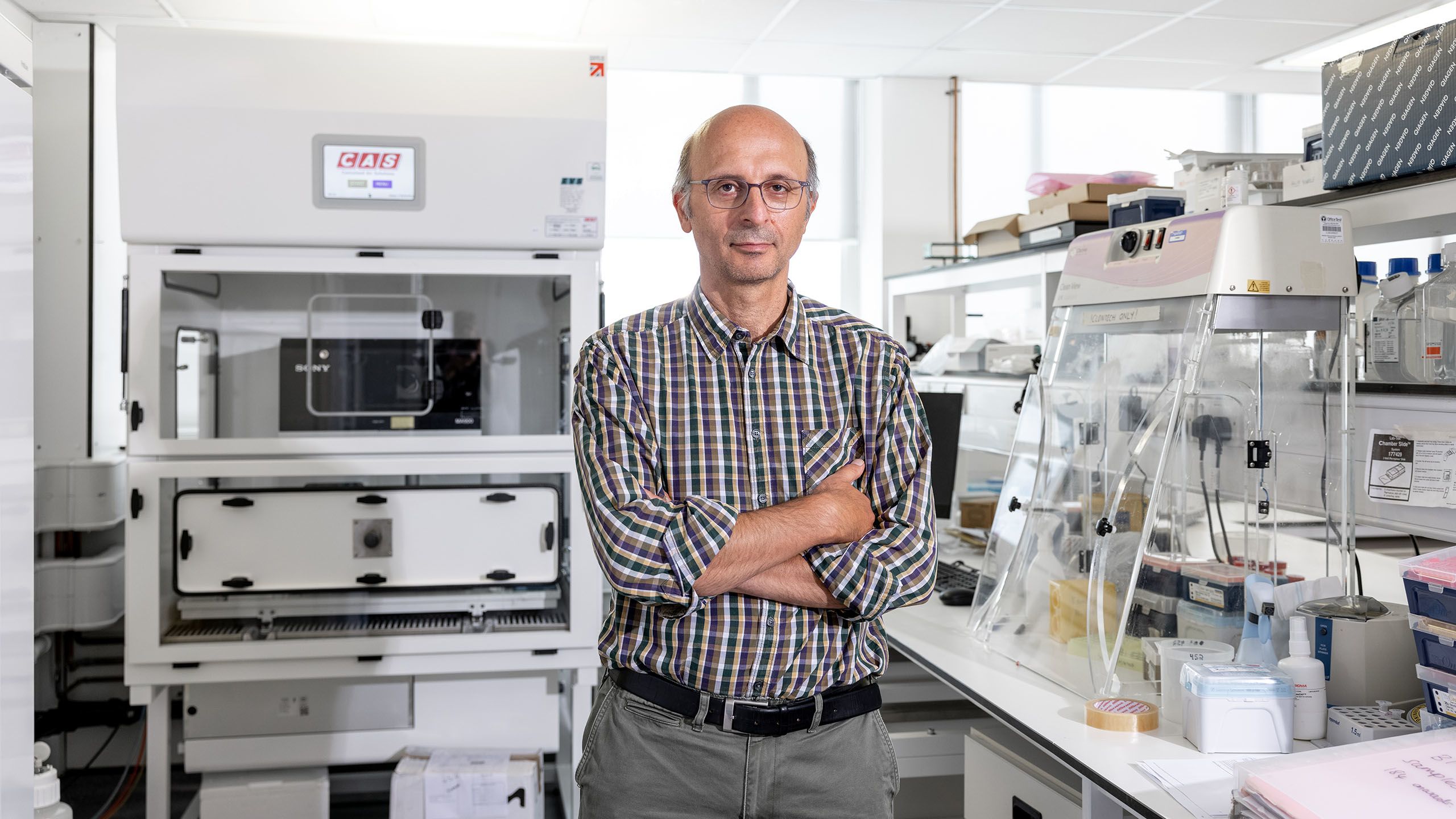
Professor Tassos Karadimitris is one of the world’s leading authorities on iNKT cells. Photo: Thomas Angus.
Professor Tassos Karadimitris is one of the world’s leading authorities on iNKT cells. Photo: Thomas Angus.
A research journey
Despite the therapeutic potential of iNKT cells, there has been much less research into their therapeutic use than conventional T cells, and they are not yet being widely harnessed for cell therapy. This is because iNKT cells are rare in the body and hard to isolate in large numbers.
Professor Karadimitris’ career helps illustrate the hard-won expertise and years of research required to deliver medical innovations of this kind.
Alongside his clinical role as a consultant haematologist, Professor Karadimitris is one of the world’s leading authorities on iNKT cells and it is his expertise in isolating them, combined with the new technique that he, clinical research fellow Dr Antonia Rotolo and colleagues have developed for producing CAR-iNKT cells, that has made it possible to begin clinically developing the new therapy. The research was funded by Bloodwise, the Imperial National Institute for Health Research Biomedical Research Centre, and Imperial Confidence in Concept.
Professor Karadimitris’ career helps illustrate the hard-won expertise and years of research required to deliver medical innovations of this kind. His research career began as a PhD student at Memorial Sloan Kettering, New York, with Professor Lucio Luzzato. Professor Karadimitris developed an interest in iNKT cells, which he believed played a role in the haematological disease paroxysmal nocturnal haemoglobinuria. His work here took place next door to the lab of Professor Michel Sadelain, who he describes as “one of the gurus of CAR technology.”
I run a clinic for patients with blood cancers and that provides the impetus: seeing patients and our failures often to provide meaningful treatments. That really comes into our lab and infuses into our scientists.”
Professor Karadimitris went on to work in Oxford with Professor Enzo Cerundolo and then Cambridge with Nobel laureate César Milstein. “By the end,” he says, “I achieved something very important – the development of tools to allow the study of the newly described iNKT cells.”
After joining Imperial as a clinical senior lecturer, he continued to research the role of iNKT cells in immunology and in haematological diseases but faced several early failures. “As early as 2012, we had evidence that they could be therapeutically developed to prevent acute graft-versus-host disease, a fatal complication of stem cell transplantation. However, we failed repeatedly to obtain funding to proceed with clinical development of this concept. At the same time, as CAR-T immunotherapy was coming to prominence, we thought that it would be a good idea to combine iNKT with CAR.
“We had a brilliant clinical research fellow in Antonella Rotolo and she pursued that as a PhD project. Three years ago, we published our results, which are the foundations of the work we are now developing.” A paper by Dr Rotolo, Professor Karadimitris and colleagues has been published in the journal Cancer Cell.
Professor Karadimitris says that clinical work with cancer patients is a driving force behind his team’s success. “At the moment I am running a clinic for patients with blood cancers. Of course, that provides the impetus, that’s where it all stems from: seeing patients and seeing their needs, and our failures often to provide meaningful treatments. That really comes into our lab, hopefully infuses into our scientists, who are a mixture of clinical academics, scientists, students of all forms, from different social and ethnic backgrounds. That’s the wonderful thing about it and the recipe for success.”

Hammersmith Hospital, where Professor Karadimitris works as a consultant haematologist. Professor Karadimitris says that his work with patients provides the impetus for his research.
Hammersmith Hospital, where Professor Karadimitris works as a consultant haematologist. Professor Karadimitris says that his work with patients provides the impetus for his research.
Future challenges
Cell therapy, which includes immunotherapies and other treatments that involve manipulating human cells, was until recently considered unproven. But evidence is mounting that cell therapy has therapeutic potential for a range of conditions.
“A few years back, I was one of the sceptics about cell therapy,” says Professor Karadimitris. “But the proof is in the pudding. We see patients being cured. When we see patients being cured by a type of therapeutic modality, then we should believe that we can deliver it at the wider scale; and that’s the challenge now, the wider scale of delivery of such therapies. And that’s where iNKT immunotherapy really comes to the fore. Because we will be able to prepare it in advance in large batches, iNKT immunotherapy will hopefully become available through the NHS at a low cost."
For some cancers like blood cancers it could be almost transformative, or incremental in a way that is very meaningful. For solid tumours, I think the clinical progress will be relatively fast because they are more common cancers so there will be more patients available to treat in clinical development and testing.
A key challenge will be the use of immunotherapy for solid tumours, which are less easily targeted by immune cells. “There’s still no definitive evidence that we can achieve as much with solid cancers as we are achieving in blood cancers,” Professor Karadimitris cautions. “Conventional T cells will not do that very well, but unconventional cells like iNKT cells are well known for the ability to infiltrate peripheral tissue where most solid tumours arise. From that aspect I’m optimistic that iNKT cells can deliver better outcomes than T cells.”
“For some cancers like blood cancers it could be almost transformative, or incremental in a way that is very meaningful. For solid tumours, I think the clinical progress will be relatively fast because they are more common cancers so there will be more patients available to treat in clinical development and testing. I would be optimistic that within the next few years we will be seeing meaningful cellular immunotherapy approaches for patients with solid tumour cancers.”
Professor Karadimitris’ lab has received funding to explore applications of CAR-iNKT therapy to HIV and is at the early stage of investigating its potential for autoimmune diseases. “We have early encouraging data to show that, based on their inherent biological properties, iNKT cells would be ideal for developing a cell therapy to treat HIV infection. Our data so far is at an early stage, we’re very excited that we’ve just now been awarded additional funding so we can test what we have developed in the lab in an in vivo setting in an animal model of HIV infection. We also have plans to develop iNKT cell immunotherapy for autoimmune diseases.”

Dr Hongwei Ren, a research fellow in Professor Karadimitris' lab, uses CAR-INKT cells to kill HIV infected cells. The team is beginning pre-clinical research into the therapy's potential application to HIV.
Dr Hongwei Ren, a research fellow in Professor Karadimitris' lab, uses CAR-INKT cells to kill HIV infected cells. The team is beginning pre-clinical research into the therapy's potential application to HIV.
Commercial support
The development of the new cell therapy has been supported by several years of commercial and legal work by commercialisation specialists at Imperial and reflects the resources offered by the College to support translational research and promote the commercialisation of new technologies in medicine and other fields.
Imperial helps bridge a funding gap that can hamper the development of early-stage medical innovations through the Imperial Confidence in Concept scheme, which offers researchers funding to identify proofs of concept, and Apollo Therapeutics, a biopharmaceutical company co-founded by the College that recently received over £100 million funding from predominantly US-based investors to support the development of new medicines in partnership with Imperial and other universities.
The development of the new cell therapy has been supported by several years of work by commercialisation specialists at Imperial and reflects the resources offered to support translation and commercialisation.
Specialist support is offered by Enterprise, a 130-strong team of experts in industry partnerships, commercialisation, and entrepreneurship, who work with researchers and students at the university to create technologies, ventures and projects that make a real-world impact.
The team helps companies access Imperial’s expertise and resources in a range of ways including research partnerships, consultancy, technology licensing, and co-location. Arovella Therapeutics has benefited from a licensing deal and collaborative research, and has engaged Professor Karadimitris as an advisor through Imperial Consultants.

This feature was produced by Imperial's Enterprise Division. The Enterprise team helps businesses to solve their challenges by accessing Imperial's expertise, talent and resources, and helps staff and students find new ways to turn their expertise into benefits for society.
