 Systems Modelling and Simulation is a discipline that relies on creating a suitable computerised representation (Computer Model) of a system, with all or a subset of its properties, which is then iteratively executed over time (Simulated) to study the behaviour of the system, with the aim to better understand the interaction of its parts, as well as the whole. Systems Modelling and Simulation techniques are widely used in fields as varied as engineering, computer science, physics, chemistry, biology, economics and medicine. Advances in Systems Engineering, Software Engineering and computational platforms have enabled the real-time or near real-time modelling and simulation of complex systems for optimisation, prediction and what-if analyses.
Systems Modelling and Simulation is a discipline that relies on creating a suitable computerised representation (Computer Model) of a system, with all or a subset of its properties, which is then iteratively executed over time (Simulated) to study the behaviour of the system, with the aim to better understand the interaction of its parts, as well as the whole. Systems Modelling and Simulation techniques are widely used in fields as varied as engineering, computer science, physics, chemistry, biology, economics and medicine. Advances in Systems Engineering, Software Engineering and computational platforms have enabled the real-time or near real-time modelling and simulation of complex systems for optimisation, prediction and what-if analyses.
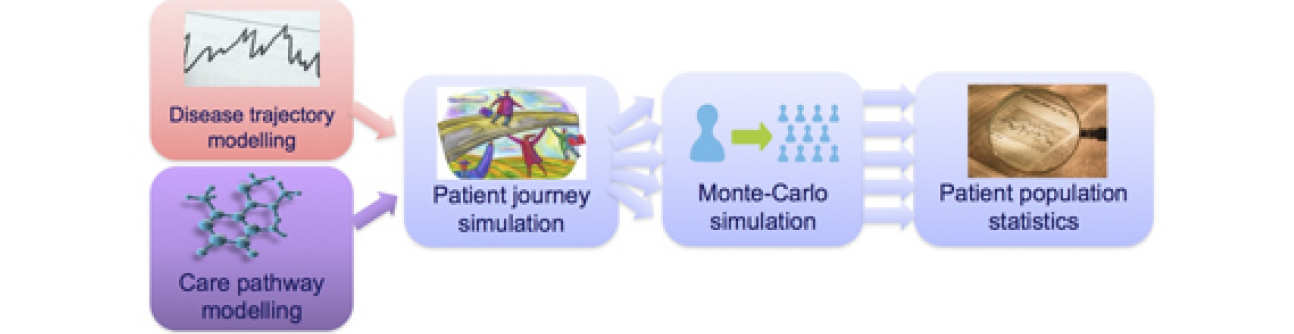
We are using mathematical modelling and computer simulation to study patient journeys across an entire integrated care pathway, from the management of health in the home to acute care and specialist services. Models of disease trajectories and discrete event simulation of care pathways are combined to generate stochastic modelling of patient journeys, in order to study and explore possible ways of improving patient and clinician experience, as well as outcomes.
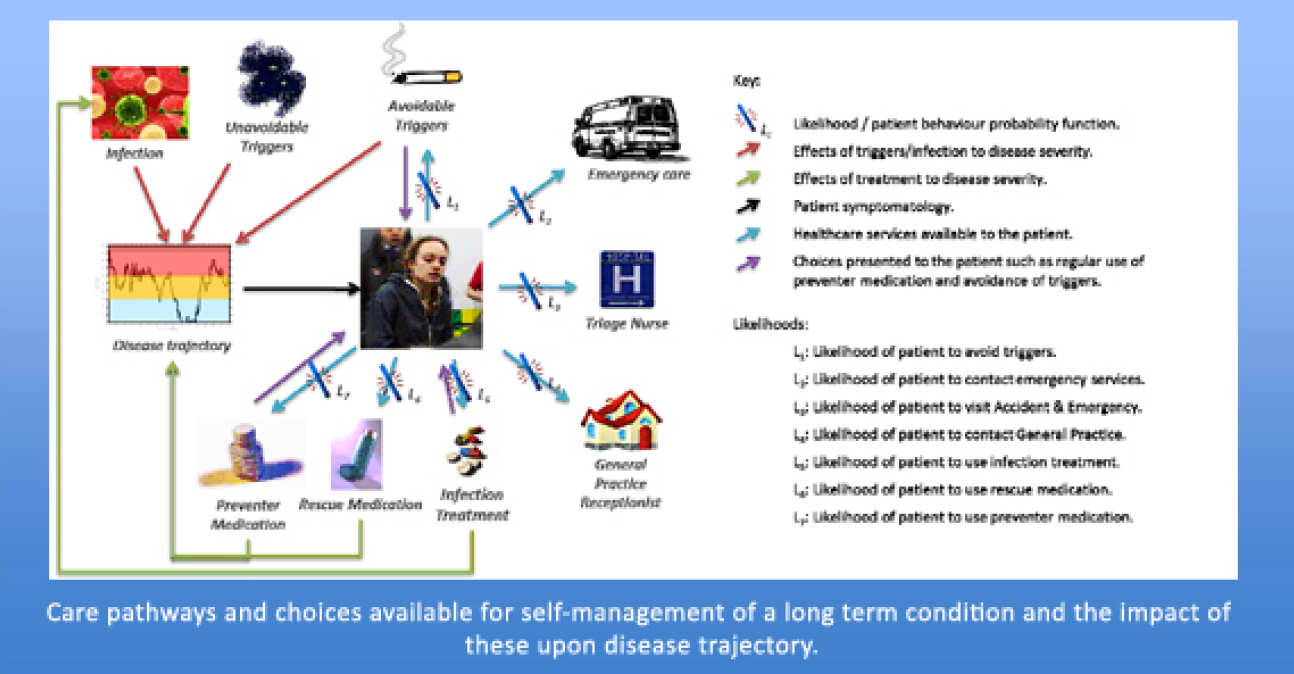
Our particular emphasis is on patient groups with complex care needs. Since the complexity of the care pathways presented by these patient groups is related to an intricate and interlinked set of psycho-social issues, lifestyle factors and provision of care between multiple separate health care providers and multidisciplinary teams (MDT), we aim to model the entire integrated care pathway, simulating patient behaviour and identifying possible opportunities for improved delivery of care and improved MDT training.
Current projects
Current projects
The Research Project
What's the problem area?
This work is part of a larger research effort concerning integrated care pathways. Here we are concerned with mathematical modelling and computer-based simulation of patient journeys, with particular emphasis on patient groups with complex care needs, such as: paediatric asthma; paediatric sickle cell disease; type II diabetes mellitus and elderly, frail patients.
Patient journeys are driven from underlying disease trajectories and are simulated using discrete event simulation. Population statistics are studied using Monte-Carlo simulation. The complexity of the care pathways presented by the patient groups under consideration is related to a variety of psycho-social issues, lifestyle factors and provision of care between multiple, separate health care providers.
Main Objectives
Our ultimate aim is to support service transformation and education through the innovative use of simulation.
We aim to model the entire integrated care pathway, from management of health in the home to acute care and provision of specialist services, as well as simulate patient behaviour.
Entire integrated care pathway models will be used to assist in the assessment and design of integrated care pathway intervention projects currently underway in Inner North West London.
Current Progress
Final models have been designed and built alongside existing integrated care pathway intervention projects. Intervention patient population statistics will be used to tune models to mimic the given populations. Once the method has been proven, the project can align more closely with intervention project groups and assist with the assessment and design of integrated care pathway interventions.
Publications & Other Outputs
Posters have been presented at:
- 7th Institute for Mathematics and its Applications (IMA) International Conference on Quantitative Modelling in the Management of Health and Social Care, 25th – 27th March 2013, London.
- European Care Pathway Conference, 20th – 21st June 2013, Glasgow.
Previous projects
Previous projects
- Imperial College Electronic Surgical Checklist (ICeS-checklist)
- Stroke Unit Purposely Constructed Resources for Training and Simulation (SUPPORTS)

The Research Project
What's the problem area?
In 2009, following the worldwide success of the WHO Safe Surgery saves lives safety checklist, the National Patient Safety Agency modified the WHO’s original checklist and mandated its use in NHS hospitals in England. The WHO Safe Surgery Checklist is now part of routine practice in all theatres today. Over the last few years, some international centres have been effectively modifying the checklist to meet their own practices. Our project aim was to develop this concept further by modifying the checklist dynamically through an iPad App, which electronically customises the checklist to each patient’s medical and surgical needs and has ability to record and share data.
Main Objectives
Design, implement and analyse the feasibility of the app through simulated surgical scenarios.
Collect preliminary results by piloting the initial app and conducting semi-structured interviews with bariatric surgeons and anaesthetists as requirements of new design.
Develop and implement the app to be able to customise and personalise the checklist, record data locally, as well as to be able to synchronise to remote server for data transmitting and sharing.
By applying a 3-tier architecture to our system, we aimed to make the most of centralised data and data in demand, establishing a secure data communication between the client-server-data-repository.
Current Progress
A final version of the App was trialled both in a simulated setting, as well as in the Bariatric surgery unit at St Mary's Hospital
Publications & Other Outputs
Poster was presented at:
-
7th International meeting on Behavioural Science Applied to Surgery and Acute Care Settings, 18th – 19th October 2013, Stockholm.
The Research Project
What's the problem area?
Stroke involves a disruption of blood supply to the brain, causing cell death. The disruption can be due to a blockage of an artery (ischaemic stroke) or due to the bursting of an artery (haemorrhagic stroke). It is estimated that there are over 100,000 strokes per year in UK with more than half of patients having disability arising from the stroke. Stroke units save lives: stroke patients in general wards have 14-25% higher mortality than patients in dedicated stroke units. These are the main causes for ischaemic stroke: cardioembolic, actherothromboembolism, small vessel disease and haematological disease.
Main Objectives
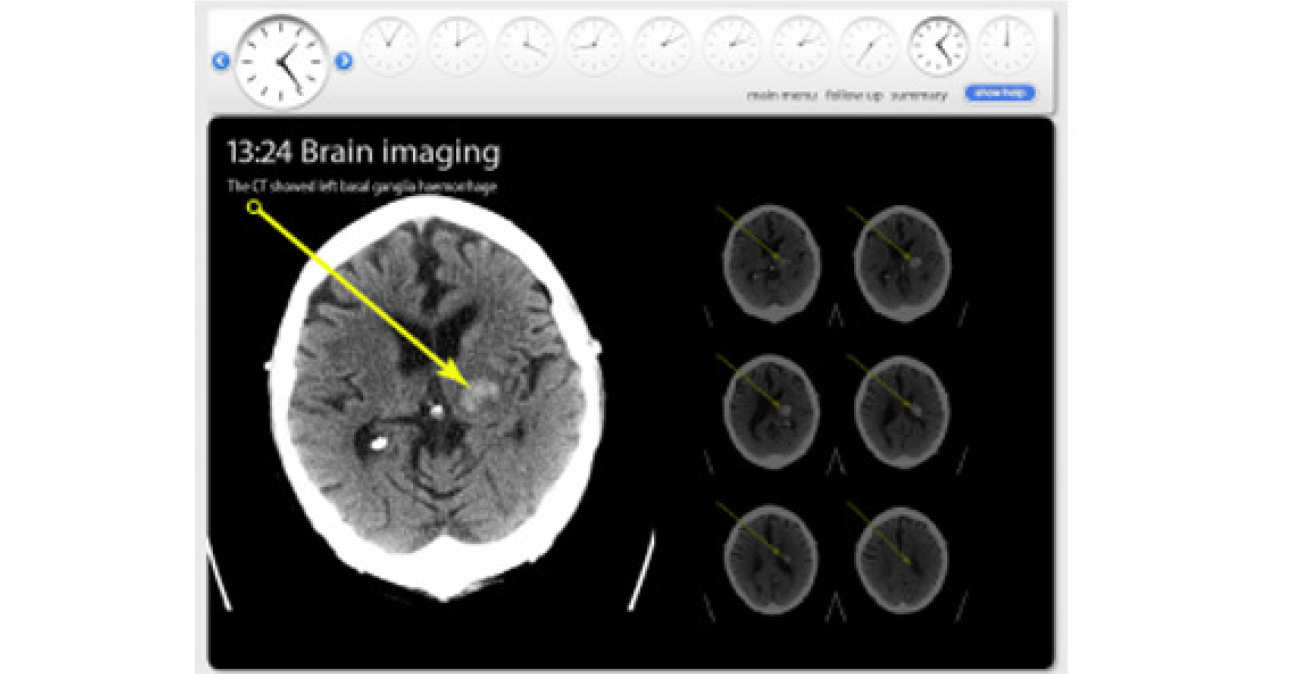
The primary aim was to implement an e-learning package to ensure that the workforce in the London Hyper-Acute and Stroke Rehabilitation Units are fully trained using a wide range of teaching resources. The electronic-learning module shown is an edited version of a module that was deployed to enable all members of the multi-disciplinary team have access to training material. The module was developed in conjunction with stroke physicians, nurses, speech and language therapists, physiotherapists and occupational therapists on the ward. There was also input from the London Ambulance Service and GP’s to ensure that those health-care workers who may come in contact with stroke outside the hyper-acute setting can understand the issues relating to stroke diagnosis and treatment in the hospital.
Current Progress
Permission was obtained to film patients and staff throughout their journey on the stroke pathway. This involved the initial emergency assessment, imaging and access to the patient’s medical record. These resources were then edited into ‘scenarios’ which the staff used to help understand various aspects of acute stroke diagnosis and management. The scenario shown is for a brain haemorrhage. A total of nine distinct scenarios were produced and validated.
Publications & Other Outputs
Poster was presented at:
-
6th UK Stroke Forum, 29th Nov – 1st Dec 2011, Glasgow.
General Enquiries
For further information on our research projects or current opportunities, please contact:
Professor of Surgical Computing and Simulation Science
Professor Fernando Bello
f.bello@imperial.ac.uk
+44 (0)20 3315 8231
