Fighting Ebola
Imperial scientists, in the lab
and on the ground, are working
to defeat Ebola

Ebola. The word alone implies a death sentence, and for 11,310 people in West Africa between March 2014 and April 2016 that is exactly what it was. In 2014 the world wasn’t ready: previous outbreaks, such as in DR Congo in 2012, had caused a maximum of 36 deaths. Being unprepared was part of the problem, but the sheer scale of the disaster means that Imperial scientists are more determined than ever to make sure the lessons are learned.
One of those at the very forefront of the battle, both then and now, is clinical research fellow in the Department of Medicine, Dr Nathalie MacDermott. She travelled to Liberia in early July 2014 with one of the first disaster response teams, through the charity Samaritan’s Purse.
“At that time no-one in the international community was really concerned,” she remembers.
“The World Health Organisation (WHO) and other experts were still saying it would burn itself out. But when we got there, Médecins Sans Frontières were already overwhelmed, and asked us to take over the treatment centres in Liberia.”
Those treatment centres had not been designed for an epidemic. “We were lying patients on the floor. It was dire. We had to knock through the partition wall of the treatment centre in Monrovia – ELWA 2 – to add beds. While we were doing that four patients died in two hours.
People were rioting outside the compound. They were afraid. They didn’t want the treatment centre there, because it would mean sick people coming.
"Ebola is a horrific, febrile illness transmitted by direct contact with the bodily fluids of infected people. There is diarrhoea and vomiting. Some people bleed from multiple sites and die from that, others have high fevers or seizures before they die.
“By the end of July the epidemic was out of control – every day people were coming from a new area, so we could see it spreading throughout the whole country. Our morgue was overflowing.”
At that point two of MacDermott’s American colleagues contracted Ebola and, subsequently, the whole team was evacuated.

We were lying patients on the floor. It was dire.
Four patients died in two hours and by the end of July it was out of control
Analysing data in real time
At the same time, Professor Neil Ferguson of the School of Public Health volunteered the services of Imperial’s MRC (Medical Research Council) Centre for Outbreak Analysis and Modelling to the WHO. In 2019 Professor Ferguson became the first Director of J-IDEA, the Abdul Latif Jameel Institute for Disease and Emergency Analytics. The J-IDEA team is expanding on the MRC Centre’s work on epidemics to include analysis of other health threats, such as those caused by conflict, natural disasters and climate change. The largest of its kind in the world, the centre analyses data in real time during disease outbreaks to help inform policy at a strategic level, working with governments, the military and NGOs .
“Our aim was to analyse how rapidly Ebola was spreading across each country and what the variations were within,” explains Ferguson, “in order to assess the incubation period, for example, and to answer specific questions such as how many beds were needed in treatment centres. The problem was, the data was incomplete, so trying to analyse the case-to-fatality ratio, for example, gave wildly diverging estimates.”
The data was so noisy and full of errors that it took time to clean up. We are developing open-source tools that can do it more efficiently
That is the problem of a disease outbreak in countries without adequate healthcare systems or accurate data recording. MacDermott describes the ‘perfect storm’ that allowed Ebola to spread so rapidly throughout Liberia, Sierra Leone and Guinea.
“The three countries border each other to the north of Liberia, and people travel across those borders all the time – for trade, for medical treatment or to visit family. There was no contact-tracing in place, nor proper burial facilities, and corpses are highly infectious.
“This part of the world had never seen Ebola before so health workers weren’t trained, and in any case there’s a lack of health infrastructure in these countries, still reeling from civil wars. Some of the areas were urban, which meant disease spread quickly.”
ELWA 2, for example, received patients from the West Point slum, with its high population density and Point slum, with its high population density and limited hygiene, such as communal latrines.
Then there were the beliefs and behaviour of the local population. “People were rioting outside the compound,” explains MacDermott.
“They were afraid. They didn’t want the treatment centre there, because it would mean sick people coming. There was also a widespread belief that Ebola didn’t really exist, that it was a hoax by the government to gain aid money, or that people were being taken to treatment centres for organ harvesting. In West Point, families were taking sick relatives away from the holding centre on infected mattresses.”
Ferguson says one the biggest lessons learned by the MRC centre from the outbreak is the “importance of the behaviour of individuals in stopping the spread of a disease. Where you have distrust of authority and government, for example, imposing control can be counter-productive.” The centre, he says, has since brought social scientists into its work, to try and model behaviour. “We can’t yet do it reliably,” he says. “You can count cases of hospitalisation, but quantifying behaviour is much more difficult.”
Since the Ebola outbreak, he says, the centre has also developed more sophisticated data processing tools.
No-one thought it would cause a large epidemic. That is one lesson: don’t dismiss a pathogen because you think you know it
“The data [in 2014] was so noisy and full of errors that it took time to clean up. We are developing open-source tools that can do it more efficiently. Silicon Valley software engineers are also working on this in their spare time.” And his team is developing better criteria for resource allocation.
“The World Bank’s new pandemic emergency funding facility, backed by insurance policies, aims to improve the way money is allocated to tackle these types of epidemics. We’ve helped develop the quantitative criteria for pay-outs used by that scheme.”
Comprising around 130 staff, the centre had previously worked on SARS, swine flu and MERS (Middle Eastern respiratory syndrome) coronavirus outbreaks, but Ferguson says Ebola took them, like everybody else, by surprise. “We hadn’t done significant research on Ebola prior to 2014,” he says.
“It didn’t cause much concern. It was lethal but outbreaks had always been contained; no-one thought it would cause a large epidemic. That is one lesson: don’t dismiss a pathogen because you think you know it.”

Treatment and vaccination
The MRC centre works on the full range of infectious diseases, with the world’s biggest killers – HIV, tuberculosis and malaria – commanding the biggest research groups. “But a lot of the methods are shared with other diseases, such as Ebola,” Ferguson explains.
“Machine learning tech [where computers can learn without explicit programming] is a big thing and we are employing professional programmers for the first time. A lot of our work focuses on retrospective analysis of epidemics like Ebola.”
During a crisis there is a political desire to do something but interventions need to be effective. We need to produce cost-effective vaccines in a timely manner
The aim for both Ferguson and MacDermott is disease treatment and vaccination. “HIV and malaria vaccines are challenging to develop because of how those diseases evade the immune system,” says Ferguson.
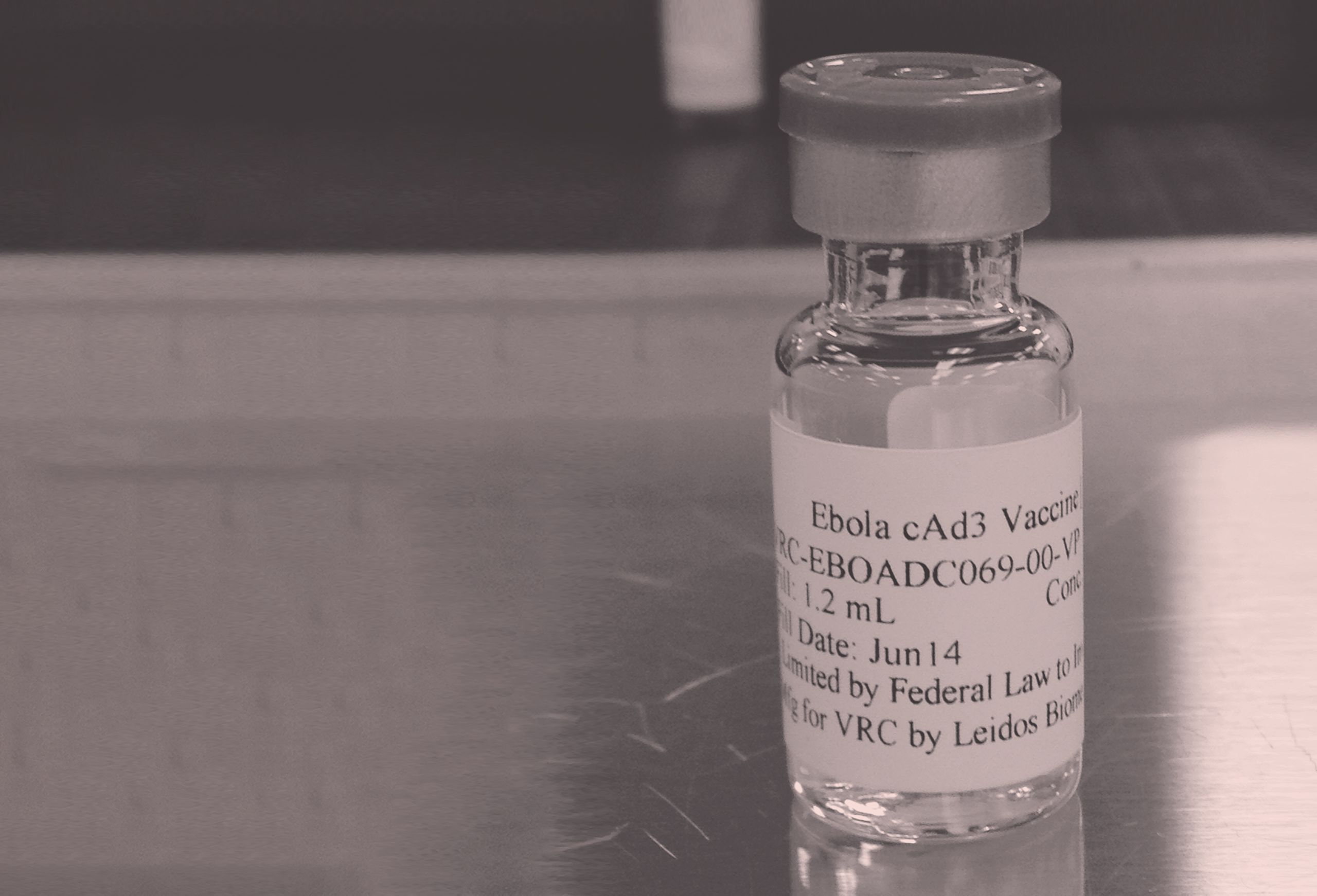
“Zika, MERS coronavirus and Ebola have a range of candidate vaccines but the problem is testing them. We are exploring how you would employ a vaccine; for example, if you stockpiled five million doses how would you deploy it in an outbreak? During a crisis there is a political desire to do something but interventions need to be effective. We need to produce cost-effective vaccines in a timely manner.”
Ironically, MacDermott says, the scale of the 2014 outbreak makes this kind of research possible in a way it wasn’t before.
"Genetic studies require thousands of participants, which we didn’t have before,” she explains.
"We’ve recruited 2,529 participants in Sierra Leone, for example: survivors – those who were living in a house where someone was sick but they themselves didn’t get sick, or controls – where no-one was sick in the house.
"We’re looking into how these people differ genetically and also if there is a genetic disposition to the kinds of problems survivors have – joint pain, eye inflammation and cataracts, even blindness, and neurological and fertility problems. We are looking at possible sexual transmission, whether how long the virus can survive in semen is genetically determined.
Differences in DNA can lead to developing treatments and identifying targets for vaccination, which can be useful in other infectious diseases
"We are just getting the results of the antibody tests – whether participants tested positive or negative for the disease antibodies – and by next summer we hope to have completed exome sequencing and genotyping. We will genetically profile all participants and study single nucleotide polymorphisms (the building blocks of DNA) to look for mutations in receptors or differences in immune response.
"This will help us to understand the virus – how it enters cells and interacts with the immune system. Differences in DNA can lead to developing treatments and identifying targets for vaccination, which can be useful in other infectious diseases such as Marburg virus disease [another virus from the Ebola family] and other viral haemorrhage fevers.”
Overall, however, the most important lesson, according to both scientists, is not a scientific one. "I hope the international community has learned the importance of responding quickly," says MacDermott, "particularly in countries where there are weak health systems"
Ferguson agrees. "There was a structural, political and logistical failure to act early enough in 2014." He says this is a lesson relevant to other diseases, so the MRC centre works on mapping geographical risk and vulnerabilities.
"Take MERS coronavirus,” he says. “There have been outbreaks in Saudi Arabia which have so far been contained. But there are migrant workers in Saudi Arabia from the Indian subcontinent – Bangladesh, for example – and were they to take it back with them to such a resource-poor country, then an outbreak there would be much more difficult to control.”

Imperial is the magazine for the Imperial community. It delivers expert comment, insight and context from – and on – the College’s engineers, mathematicians, scientists, medics, coders and leaders, as well as stories about student life and alumni experiences.
This story was published originally in Imperial/43: Winter 2017–18. It was amended on 4 November 2019.
