"The pandemic has opened our eyes..."
GP-researcher Sonia Saxena marries data and social justice in healthcare

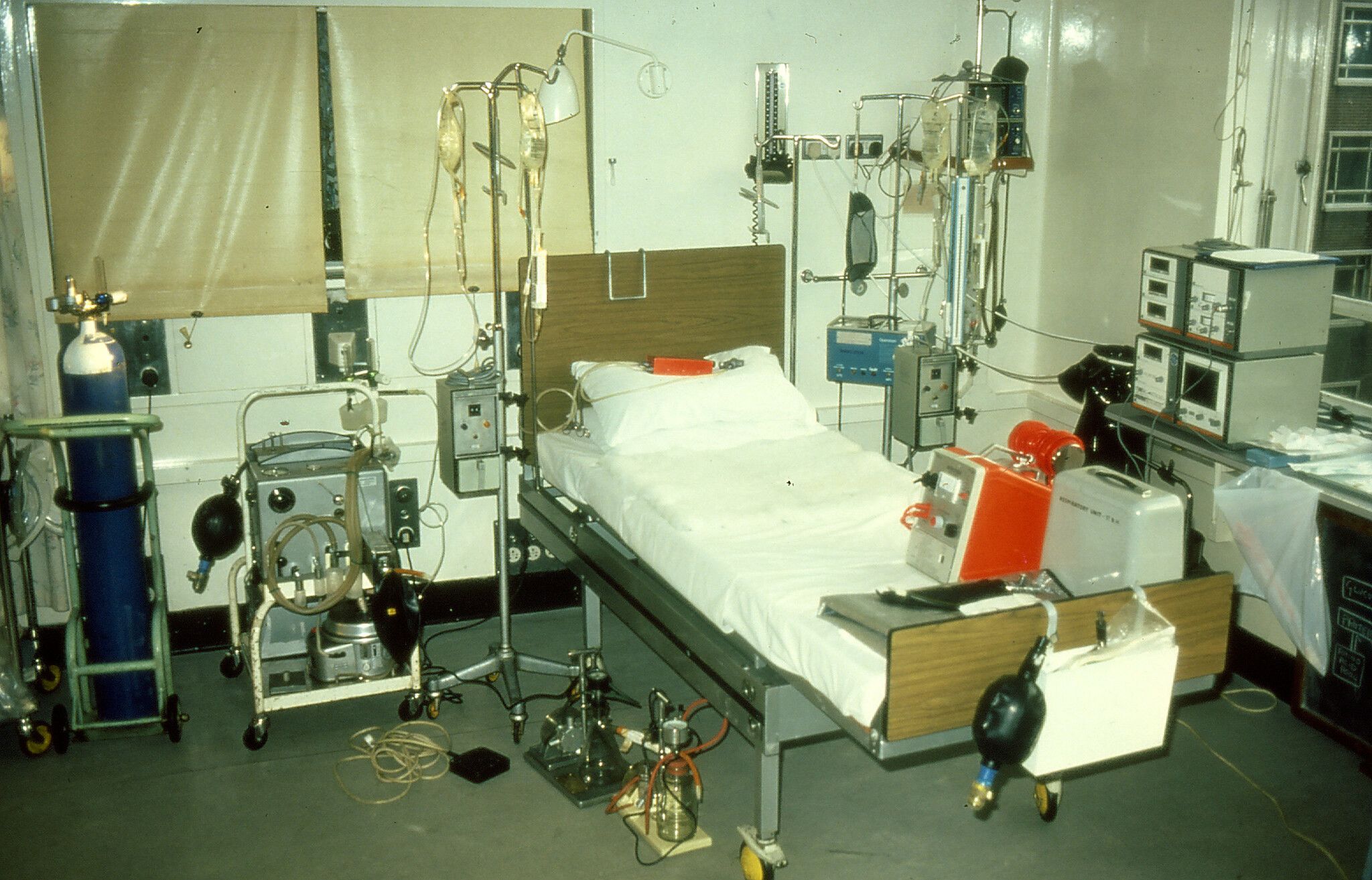
Professor Sonia Saxena’s first experience of a pandemic was in the early 1980’s as the UK’s HIV crisis was emerging. She and other staff at St Bartholomew’s Hospital, where the young doctor was training, had heard about the first cases in California.
Her formative years as a newly qualified doctor were spent diagnosing and treating patients – many of them young gay men – who would come in breathless with a new form of pneumonia, caused by the virus weakening their immune systems.
“It was so unexpected because our training had equipped us to deal with older people with longstanding medical problems like heart failure, cancers or dementia,” she says. “But instead there were these articulate young men in the prime of life with minimal signs at first such as Kaposi sarcoma, purplish blotches that appeared on the skin, but whose health rapidly took a downturn with pneumonia, weight loss or fits with so many dying right before your eyes.”
The hospital underwent a rapid period of re-organisation where it like Sonia worked in an ever-evolving war zone: “I was there on the front line. I tried to spend as much time as I could with patients, because they were often alone and very distressed."
Every week, new protocols would be introduced to adapt to changing knowledge about AIDS. Given that people did not yet understand the virus' mode of transmission, Sonia and her colleagues had policies around fastidious hand-washing and were careful when masking up and gloving up.
“We learned eventually that it was caused by a virus and transmitted through sexual contact or in blood, but there was no training and little protection, so you just had to get on with the job in hand,” she says. She recalls having a needle-stick injury while working and being invited to take a dose of zidovudine – a HIV antiretroviral drug undergoing experimental trials in the 80’s and the only treatment available at the time.
"It was a terrifying time and often you would turn up and the person you cared for the night before had died,” she remembers, “Everything evolved so fast. We often found that all of the policies we had adopted in the previous week had been thrown out and we had to adapt to new ones.”

40 years later
A new pandemic
The realities of caring for seriously ill patients became relevant more than 30 years later when Sonia served on the front line of another, much more recent pandemic.
During COVID-19, she not only worked in primary care as a general practitioner, but was also one of several GPs who volunteered to lead research and advise on health service re-organisations as part of Imperial’s COVID 19 research and policy response team throughout the pandemic.
She now leads the Child Health Unit at the School of Public Health. Her group studied both the direct effects of the pandemic on children’s health and also the indirect effects of lockdowns and school closures on their social and physical health and access to care. For example, she reported how GPs rapidly switched to a combination of face to face and remote consulting so parents could continue accessing healthcare for their children. Since COVID-19 vaccines became available, she has also written research and strategy briefings to increase the uptake of COVID-19 routine vaccinations amongst children, pregnant women and minority groups who still lack vaccine protection.
Sonia's research group at Charing Cross Hospital, 2019
Sonia's research group at Charing Cross Hospital, 2019
For Sonia, the increasing use of data in medical and health care has enabled research on a greater scale than ever possible before but the increasing use of big data is posing one of the biggest challenges facing research.
The introduction of computers into general practices was a big leap forward compared to the relatively analog systems she first worked with at the start of her career. She remembers how doctors wrote free-form entries onto paper records during the AIDS epidemic.
“We struggled to decipher paper records covered with illegible writing. The other medical staff would handwrite calculations for medication because they did not trust the still-alien technologies trickling in,” Sonia says. “So slowly, we've got to the point where everything's digitalised.”
Now, digital records are able to capture a huge breadth of a person’s medical history – from regular visits to a GP to major hospitalisations: “They contain coded information on everyday contacts that people have with clinicians.”
Sonia has invested time in ways to transform this routine data into usable numbers for observational studies that can tell us how effective healthcare interventions are, something that will only become more significant when dealing with health crises in the future.
Often, Sonia will produce her research directly with the communities she works with. Many of her investigations into COVID-19 were structured with patient participation in mind – creating a dialogue with patients and communities she has seen face to face and virtually.
“All of my research comes from questions that patients ask, regular discussions with colleagues or patient and professional groups.”
Borneo
Community healthcare in practice



In the early 1990’s during Sonia’s training at St Bartholomew’s Hospital, she completed a medical elective in Borneo. It was a trip that opened her eyes to the importance of healthcare access in more socio-economically deprived regions of the world and communities.
She spent time working in local community hospitals in Kuching and Sibu, but she would also travel up the Rejang River. The 350-mile-long river snakes across the Northwest of Borneo, along which there were many small villages and towns with limited access to healthcare.
Sonia visited longhouses – wooden buildings built on stilts sit above the river and the rainforest tree tops – in preventive outreach efforts. It was minimalist subsistence living where the community would search for food, which they would then prepare into a simple meal that they would eat together. The team were providing basic prevention interventions such as vaccinations, contraceptive care and education about how to protect themselves against malaria and waterborne infectious diseases.
On one of the visits, there was a grandmother who had developed a very large cancer on her neck, but was also the main carer of an orphan baby whose mother had died of sepsis after childbirth. She refused to be transferred to a local hospital in Sibu if it meant leaving the baby behind.
“The primary care team went to great efforts to get to the local hospital, get the surgeon to come out, make an assessment, and then over a period of time If they were able to raise the funding for her to be transferred,” Sonia says.
“I was really struck by the tenacity and compassion of primary care teams just working with the situation that they were confronted with.”
It was within primary care that Sonia was able to work closely with households she has seen go through the entire life cycle: pregnancy, childcare, adolescence, adulthood and late age. She saw how intense health crises or more protracted issues of inequality affected their lives.
An elderly woman caring for her grandchild, pictured during Sonia's medical elective in Sibu
An elderly woman caring for her grandchild, pictured during Sonia's medical elective in Sibu
A community gathered in the Philippines
A community gathered in the Philippines
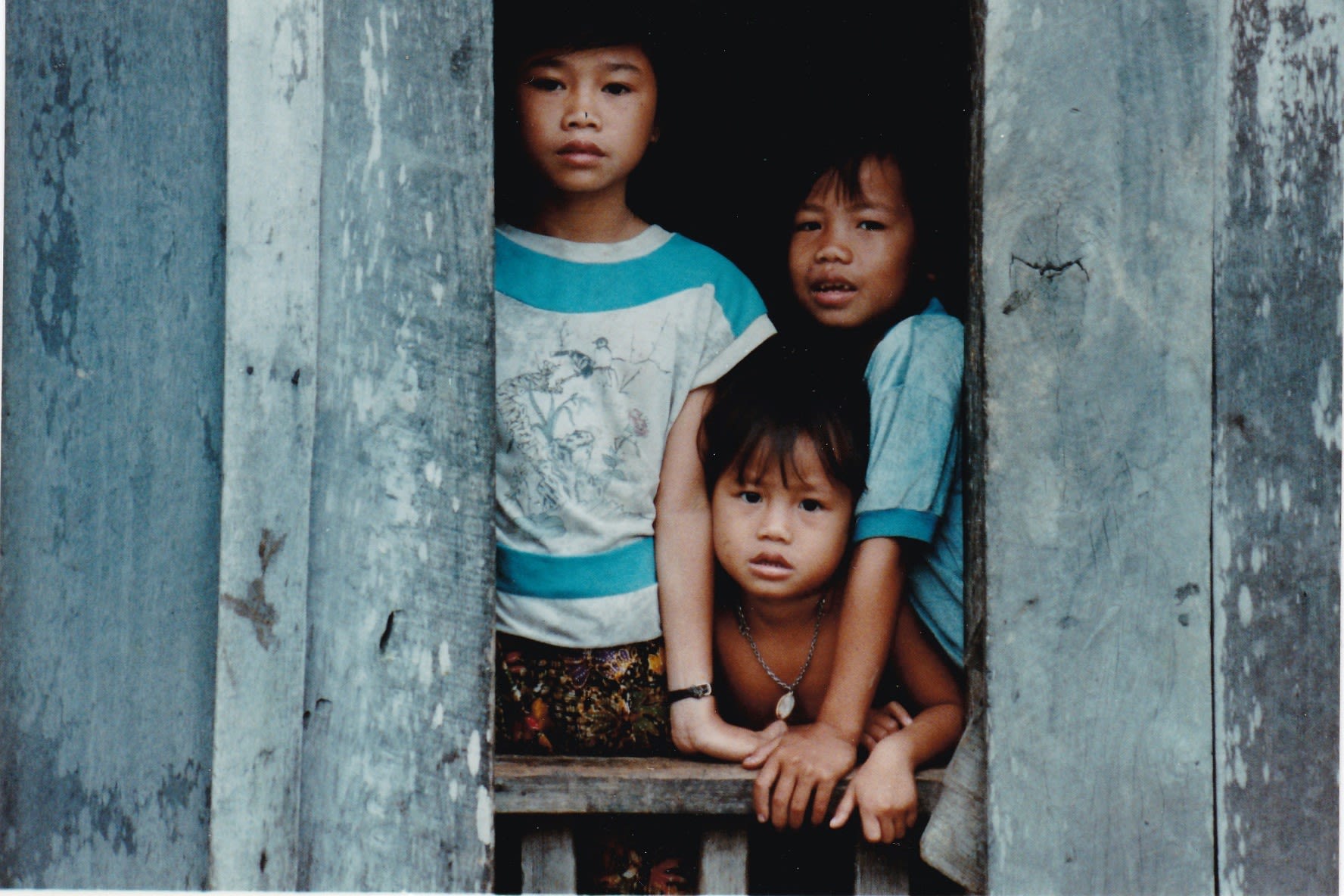
Three young children, looking outside a longhouse in Sibu
Three young children, looking outside a longhouse in Sibu
COVID-19
Exposing healthcare inequalities
In 2020, Sonia and her practice drew up protocols and trained staff on how to best protect themselves and their patients, all whilst attempting to stave off surge pressures in NHS hospitals.
“However, we also had to leverage help from the community,” she says.
Women from the local mosque helped make scrubs and masks for Sonia and her practice at the height of the PPE shortage, stitching the words ‘Angels in scrubs’ into the fabric.
Healthcare staff at Chartfield Surgery, the GP clinic where Sonia works, thanking local members of the community for donating handmade scrubs.
Healthcare staff at Chartfield Surgery, the GP clinic where Sonia works, thanking local members of the community for donating handmade scrubs.
“A bit like with HIV, many isolated people still needed human contact as well as supplies,” Sonia says, “So, my practice arranged for a volunteer workforce – including both my children who had been sent home from university – to deliver medicines to those who were shielding and offer some support with socially-distanced patients.” Volunteers befriended the elderly, helping them run errands and teaching them to send messages on their phones to their families so they could stay connected.
However, what soon became apparent Sonia was that COVID exposed existing inequalities in healthcare provision that have since widened. The pandemic disproportionately impacted the lives of ethnic minority groups – with patients from these groups dying in higher numbers and at younger ages, as numbers from the Office of National Statistics show.
The British Medical Association showed this harm extended to minority ethnic doctors and key workers who became unwell or died in the early periods of COVID, more than their counterparts.
Research from Imperial also showed that people from minority ethnic groups, especially from low-income backgrounds, also experienced the most disruption in their hospital care from cancelled or delayed appointments.
Celebrating unsung heroes
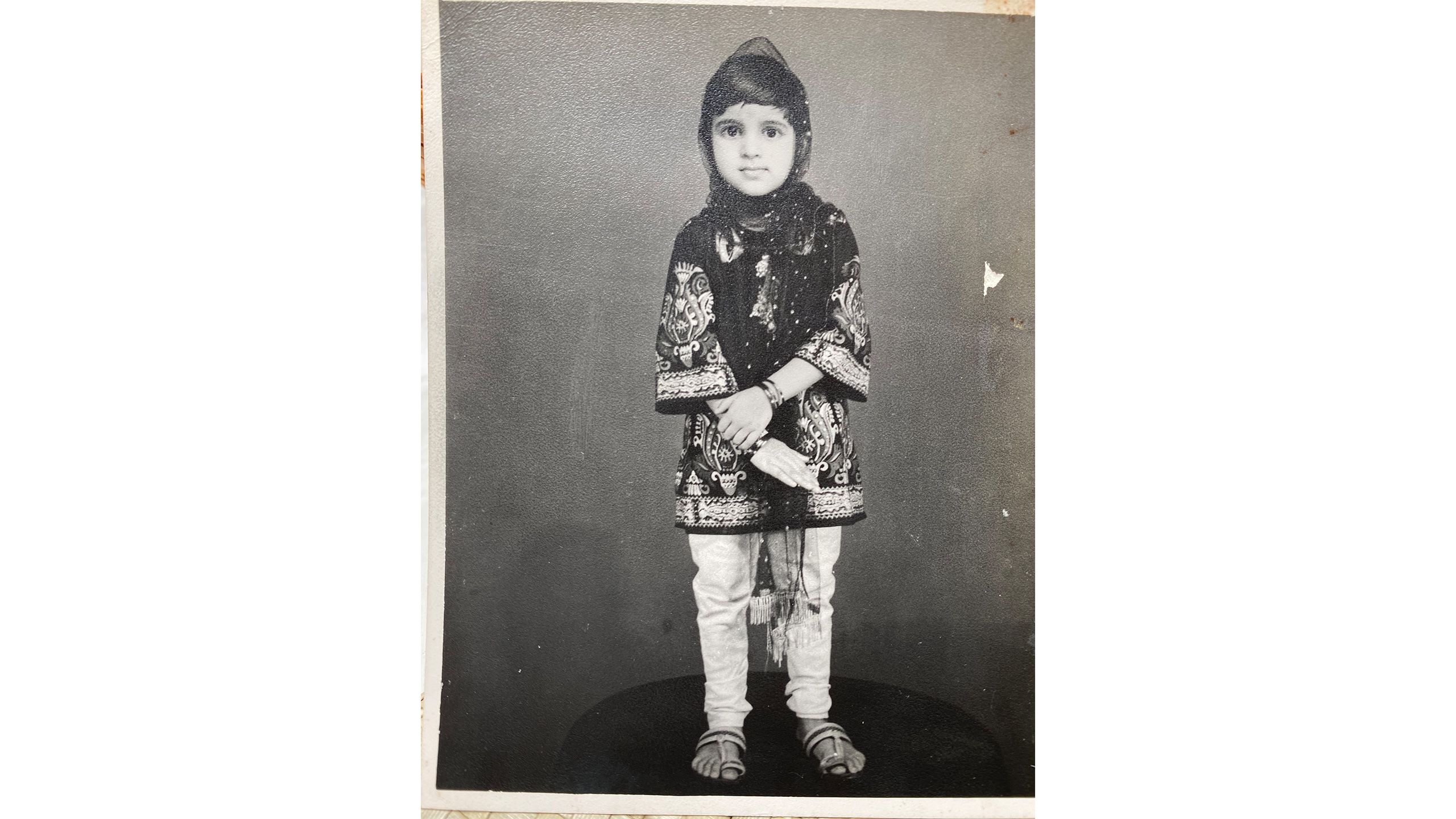
Sonia as a child, arriving in the UK from India.
Sonia as a child, arriving in the UK from India.
“I care about social justice,” Sonia says, believing that coming from a minority ethnic background herself made a difference to the issues she researches.
Her decision to become a GP in primary care had come from her time as a child, when she had just emigrated to the UK from India. She became conscious of a potential career in medicine. But her time spent training to become a doctor was challenging, she says, because of a hierarchical culture of racism and misogyny at all levels in the medical profession.
“Women were belittled… and harassed and I remember clearly that in one of the careers fairs that an orthopedic consultant said all the Pakistani and Indian doctors should get sent home but that he didn’t know who would do the work when they were,” she remembers.
Sonia’s daughter now also studies medicine in university and her mother is hopeful that she will not meet the same kind of discrimination. However, Sonia’s experiences still inform a large part of her work: motivating her to focus on healthcare for people from minority ethnic backgrounds.
The Medical Women's Federation celebrating their centenary at the British Medical Association.
The Medical Women's Federation celebrating their centenary at the British Medical Association.
She has emphasised the need to study and understand differences in health outcomes for social and ethnic groups as the inequalities during the COVID pandemic became apparent.
Data can capture under-represented people’s voice and experience, Sonia says, “but it doesn’t exist in a void; it is created – it’s fascinating how it is a language but the emphasis is made through numbers.” She warns however, that poor data and poor science can lead to misinformation and, like historical fallacies, hide important truths.
“We need to invest more in better quality data that captures the real world more accurately and rigorously and have strong governing principles to oversee the analysis so we can avoid repeating the same harmful historical legacies."
“It’s incredibly important to me that we celebrate achievements of these everyday unsung heroes like GPs while also giving a whole new generation of social activists a chance to be heard.
“The pandemic has opened our eyes to invaluable lessons and shown the way to the grand challenges of the future,” she says. “Top of my wish list is that we plan better for future pandemics, improve the quality and use of data to shed light on what we cannot see and work more directly with communities to confront discrimination and address inequalities.”
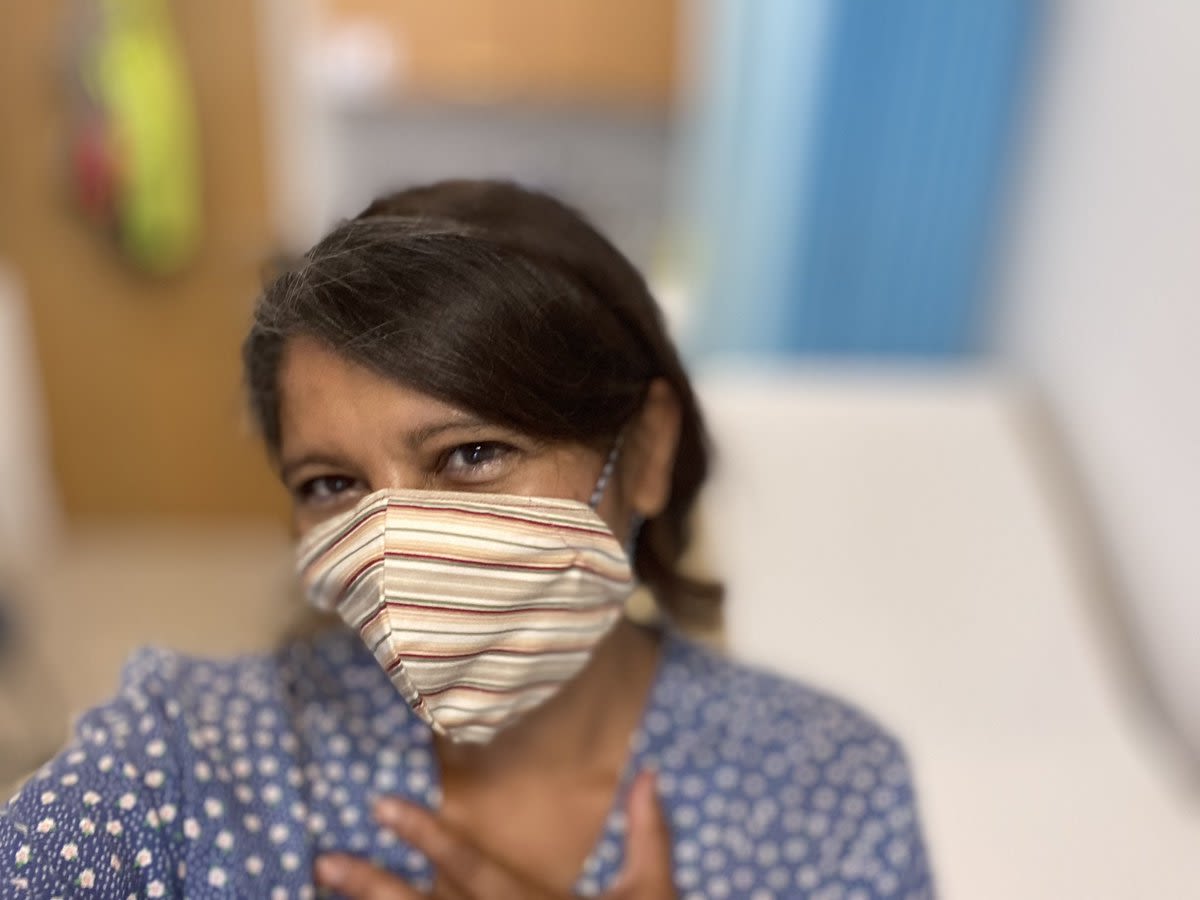
Sonia, here pictured standing in a Chartfield Surgery examination room
Sonia, here pictured standing in a Chartfield Surgery examination room