The MSk Lab has been involved for some years creating software for joint analysis and surgical planning, for the purposes of advancing science, identifying problems with an individual patient's joint and planning solutions to these problems, increasing the efficiency and effectiveness of such treatments.
The source of information for planning and analysis typically comes from three dimensional imaging, most often in the form of computerised tomography (CT), although for some tasks we also use magnetic resonance (MR) imaging. This is then processed to create three dimensional models of anatomical structures from which our software can make measurements and overlay implants and specify cuts to bones.
Some examples of the planning and analysis software created, or being created in the laboratory are:
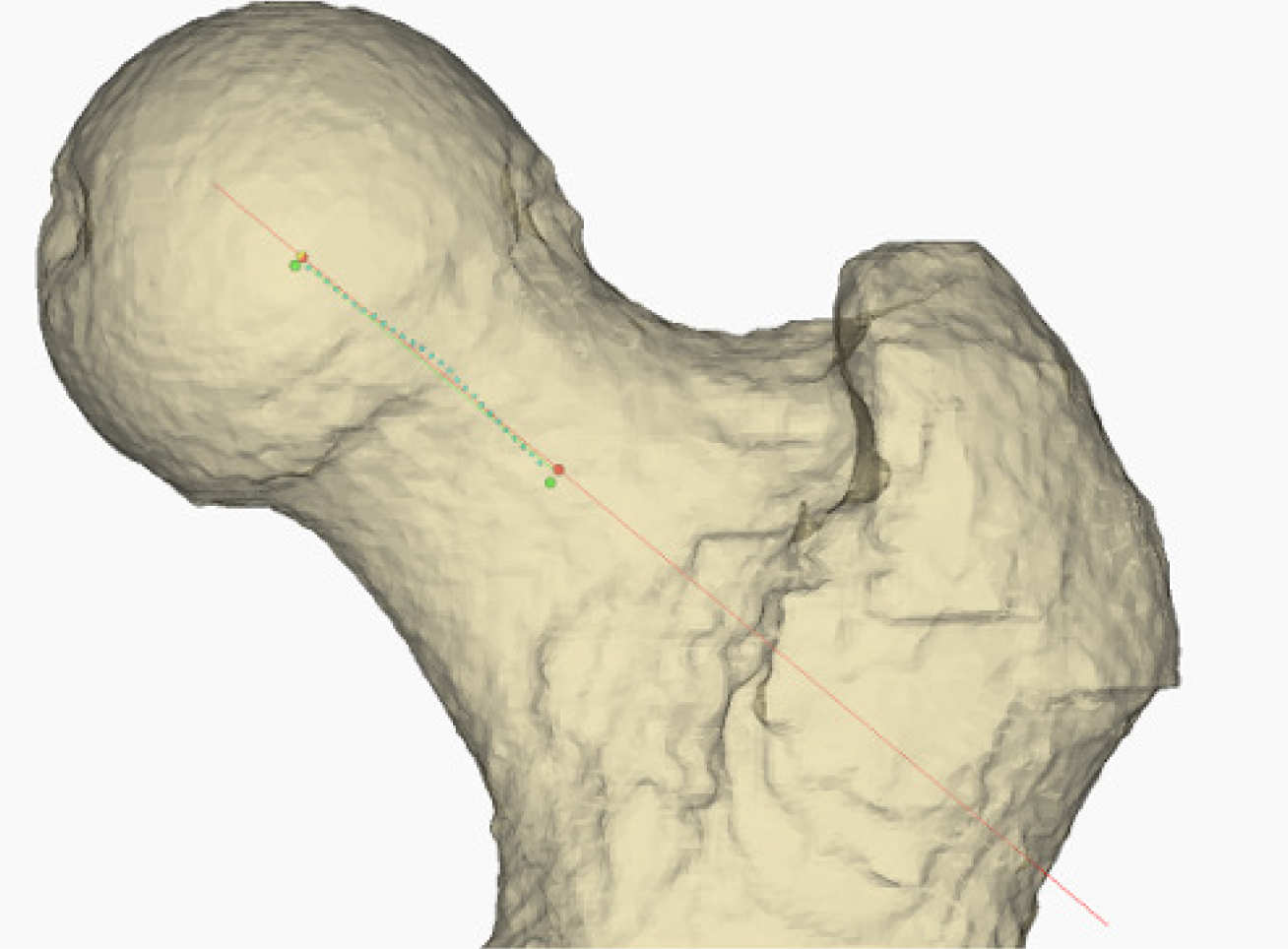
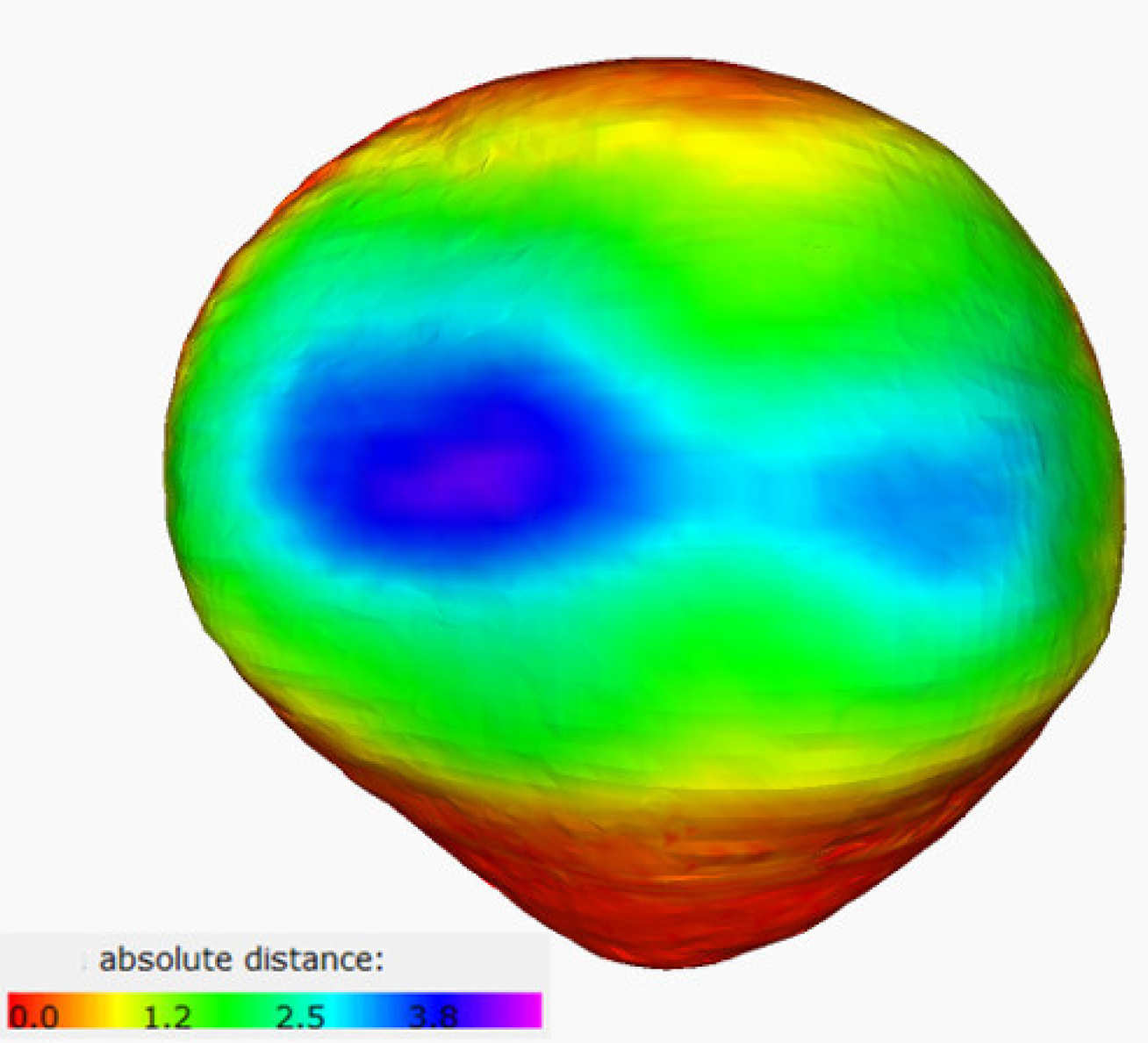
Hip impingement analysis and planning
In some patients a bump can form on the front of the femoral neck and head which can restrict the range of motion of the hip, and cause pain when attempting to overreach these restrictions. This can be surgically treated to remove the bump, however traditional methods are not always successful. We have developed software that allows the bump to be quantified and located, and for models of a more natural head and neck to be overlaid. The difference between the individual and the model can be visualised, and a program generated that enables an actively constrained robot to reshape the femoral head to a less impinging shape. We are currently extending this software to allow hip replacement surgery to be planned.
Total knee planning
In conjunction with Embody, we have created a total knee planning system that allows implants to be placed onto the femoral and tibial models of an individual. The system follows rules specified by the manufacturer to ensure that the implant is placed within safe limits. Aften planning, the geometry is used by Embody to create patient matched templates for surgery, minimising the jigs required and ensuring the surgery matches the plan.
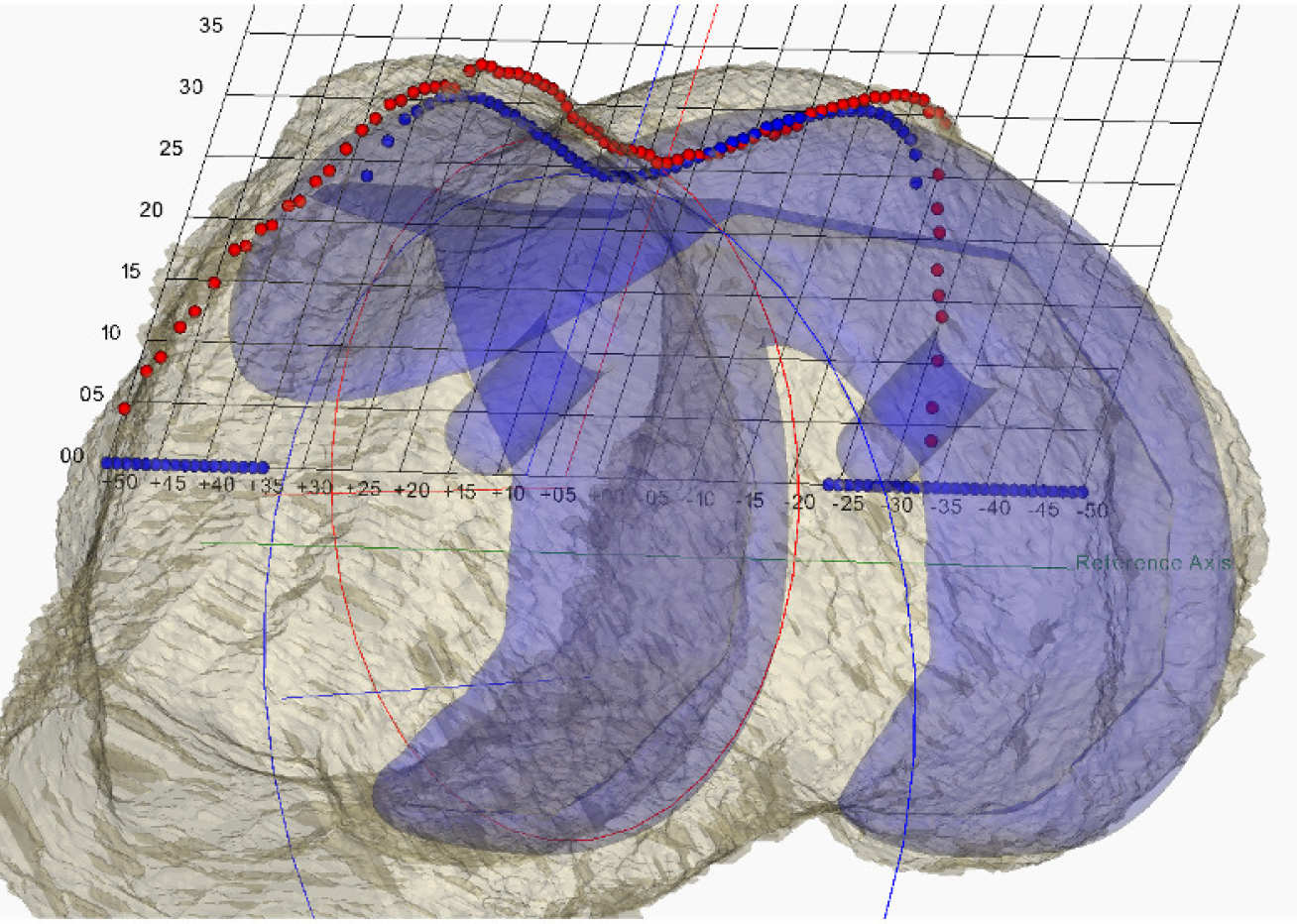
Multi-compartmental knee planning
By using small implants, much of the natural function of the knee can be preserved. In many cases a single compartment (e.g. One condyle or the trochlea) can be replaced, however, where more than one compartment is damaged, interest is growing in replacing each damaged compartments, rather than reverting to replacing the whole knee, which is detrimental to outcome. We are in the process of creating software that can plan the replacement of any or all of these compartments with small components. This is very much a novel technique, and, in parallel, we are creating analysis software to 'do the science'.
Osteotomy planning
Deformities may occur outside of a joint rather than inside of it. Such deformities may result in poor gait, or excessive wear on joints. Osteotomies may be performed on the femur or tibia, typically taking out a wedge of bone, or opening up a wedge, to realign the bone. In the MSk Lab we are developing planning software that allows an osteotomy to be specified, and the resulting bone geometry visualised. The plan can then be converted into a set of templates for the patient, allowing the surgeon to cut the osteotomy planned.
Oncology arthroplasty
It may be necessary to remove pieces of bone when tumours are discovered. The MSk Lab is developing a system that allows the tumour to be removed, plus a 'guard band'. This will leave gaps that need to be filled, either replacing bone shafts, or creating new joints. We are developing software that can specify the resections required, and the shapes of replacement components. This software is intended to reduce the necessity of amputation in cases of bone tumours, and returning the patient to a better quality of life.
Contact
Dr. Simon Harris
Research Associate
s.harris@imperial.ac.uk