25 years of groundbreaking cancer research
By Conrad Duncan
From innovative treatments to improvements in screening and diagnosis, huge strides have been made in cancer research over the last 25 years. As a major research university with experts across key disciplines, Imperial has been at the heart of many of the research challenges of the past two decades and sits at the cutting edge of new developments in treatment, prevention and diagnostics.
For the Faculty of Medicine’s 25th anniversary, we spoke to the experts behind some of the College’s biggest success stories in cancer research...
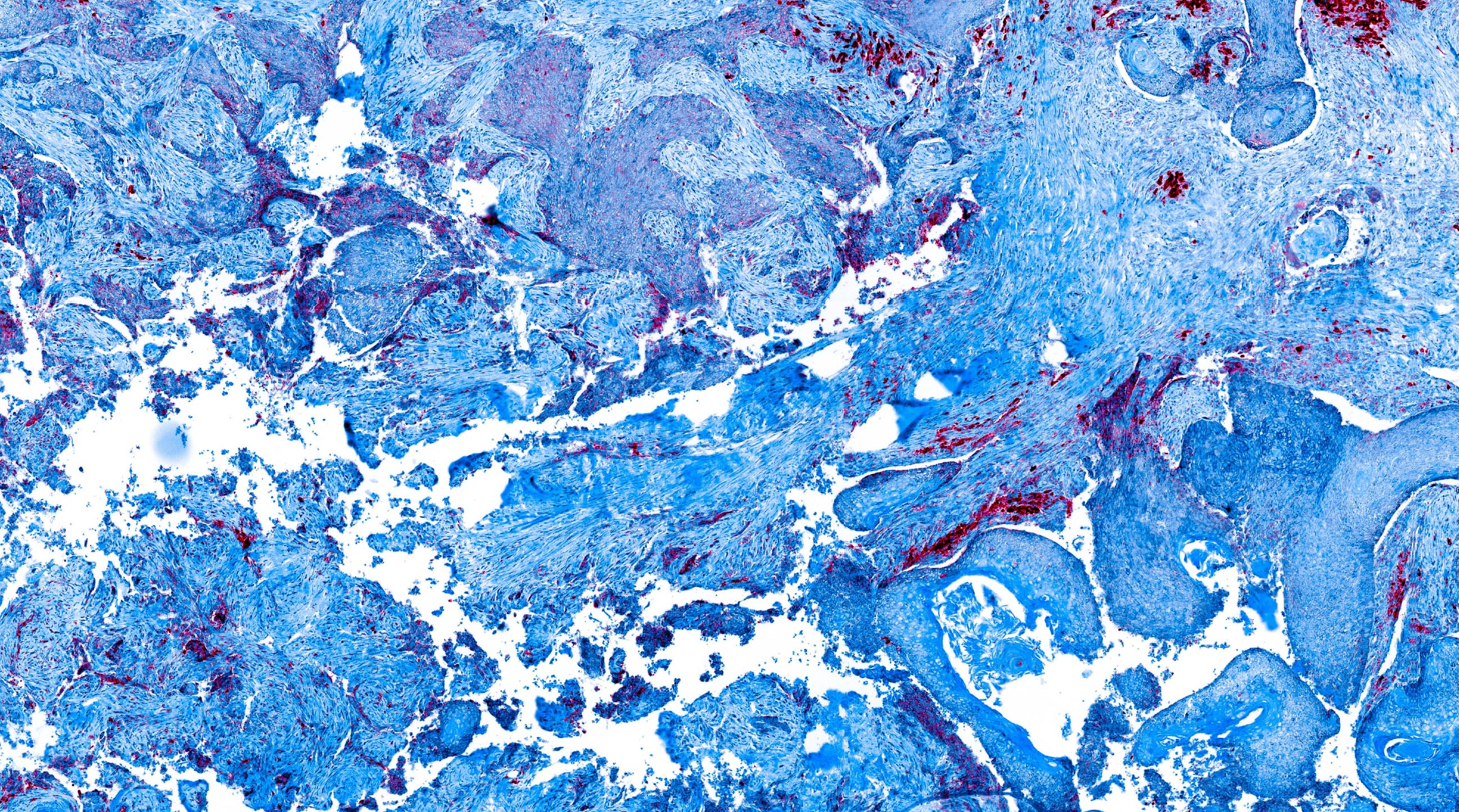
Reducing relapse rates for breast cancer

One of the major areas where Imperial has had considerable impact in cancer research, according to Professor Iain McNeish, Head of Cancer in the Department of Surgery and Cancer, has been in the field of breast cancer through work led by Professor Charles Coombes.
Alongside colleagues at Imperial, Professor Coombes worked on developing drugs known as aromatase inhibitors which block the body from producing oestrogen - with the aim of reducing relapse rates after surgery for breast cancer patients. Previously, the standard drug for hormone sensitive breast cancer cases was tamoxifen.
Research at the College led to the adoption of a drug switching treatment, where patients were treated with tamoxifen for two to three years before switching to an aromatase inhibitor called exemestane.
“One of the reasons for the switch was that blocking oestrogen production in the body can have negative effects, particularly on the bone as it can cause fractures,” Professor Coombes explained. “Tamoxifen on the other hand strengthens the bone - so we felt that by giving them two years of tamoxifen to start and then the aromatase inhibitor, we would counteract the effect of fractures. That was, in fact, what we found.” In trials, this treatment strategy was shown to improve overall survival of breast cancer patients for at least five years post-switching. It also had a secondary effect of reducing side effects such as bone fractures. It became the standard recommendation in treatment guidelines for breast cancer worldwide.
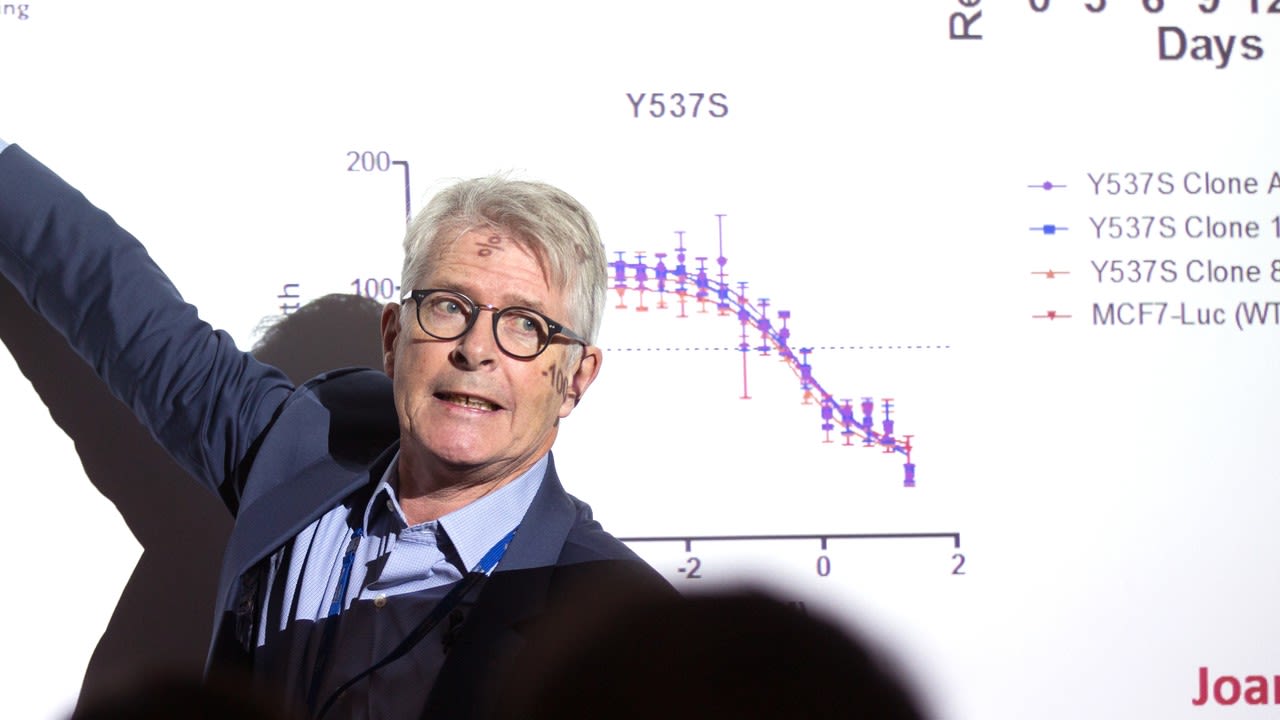
In recent years, Professor Coombes’ work has focused on countering resistance to cancer treatments through inhibiting an enzyme called CDK7, which was found to be a major cause of resistance to breast cancer treatment. Imperial researchers from the College’s Departments of Chemistry and Surgery & Cancer, including Professor Simak Ali, Professor Anthony Barrett and Professor Matthew Fuchter, worked on producing a compound to inhibit CDK7 which could be taken in tablet form. The drug (samuraciclib), which was developed with Carrick Therapeutics, received Fast Track designation from the US Food and Drug Administration last year and is currently in phase three trials in the US. It is hoped that the drug will improve outcomes for breast cancer patients, with research findings so far suggesting that in patients with metastatic disease, the compound, combined with hormonal treatment, can lead to very long remissions. “The big phase three trials that are ongoing in the States will tell us whether our hypothesis is correct,” Professor Coombes said.

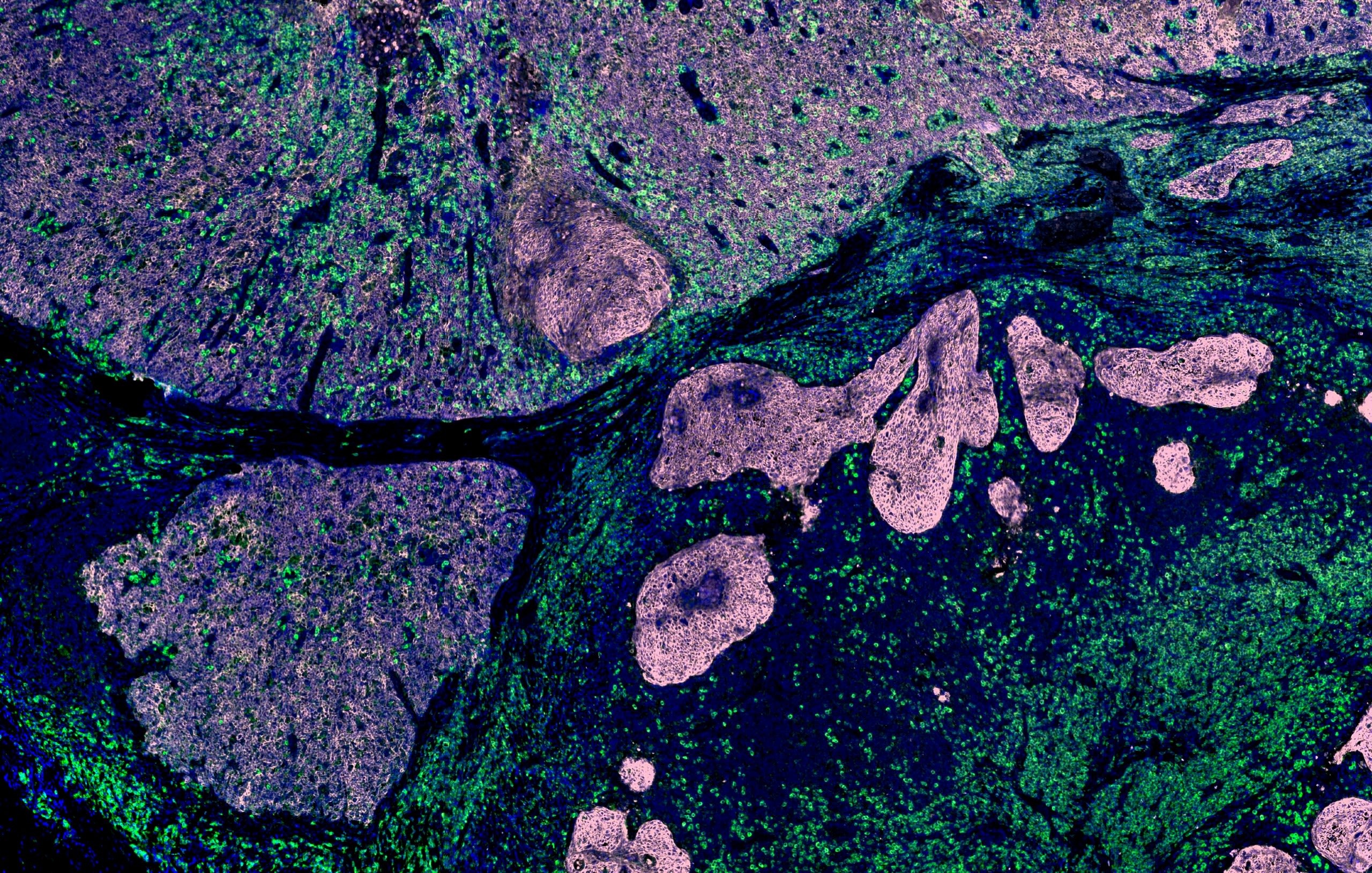
Life-changing improvements in care for chronic myeloid leukaemia
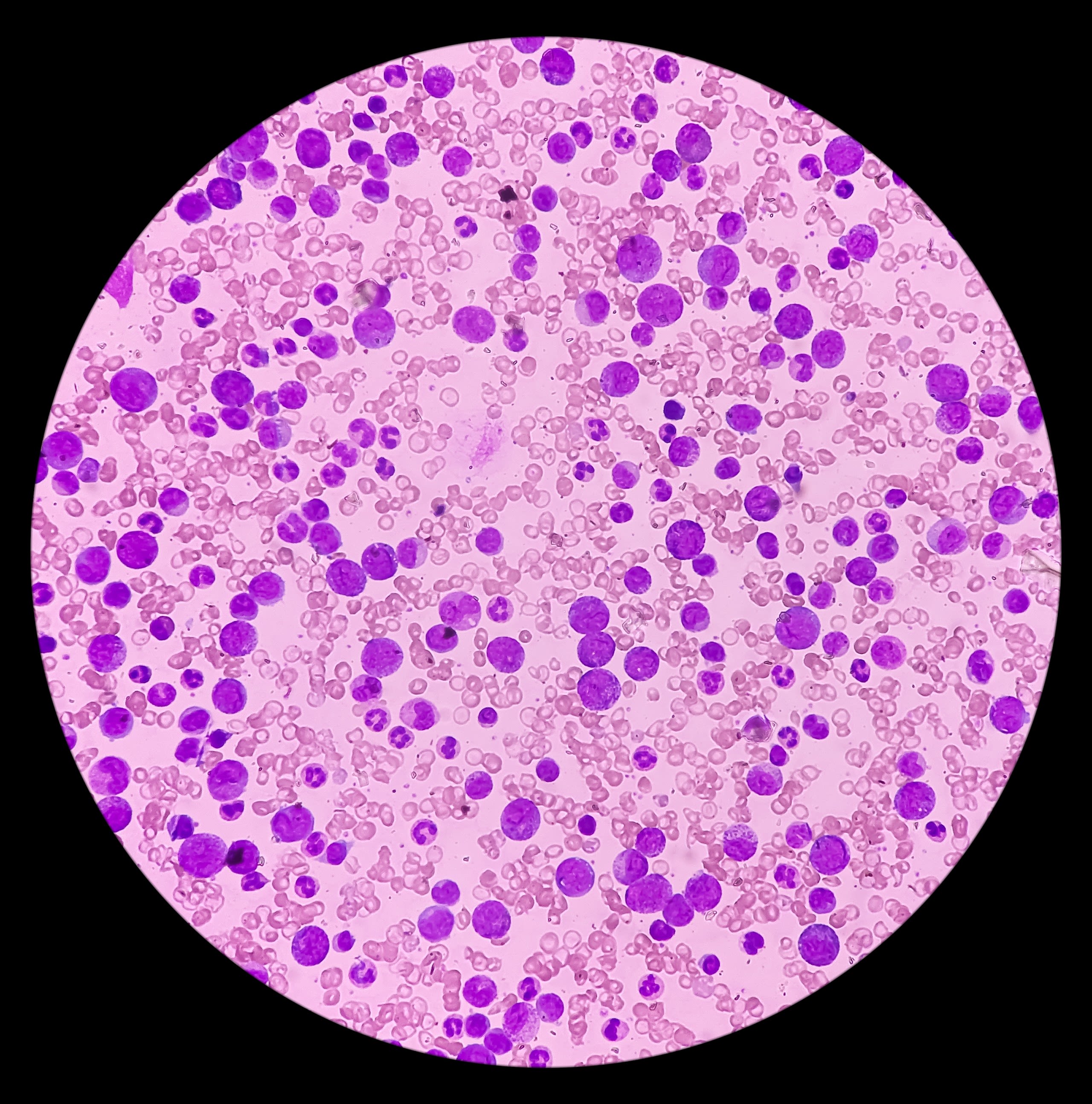
The improvement in outcomes for patients with chronic myeloid leukaemia (CML) is one of the most significant advances in cancer research over the last 25 years. It is also an area where Imperial has played a key role in improving patient management.
Professor Jane Apperley has worked on improving treatment for CML, alongside the late Professor John Goldman, since the 1980s. She explained that until the late 1990s, CML was a “mean disease” for patients. If someone was diagnosed with the condition, they could be treated with standard chemotherapy to allow them to return to normal daily life, but at an unpredictable point, their disease would inevitably worsen into a more aggressive form called blast crisis. “The patient has no idea from the moment they're diagnosed whether that's going to happen next week or in 20 years,” Professor Apperley said. “And once it gets to blast crisis, there is no cure whatsoever. There's no treatment and a death follows very quickly.”
The change in outcomes for patients since then has been transformative. All newly diagnosed patients now receive highly effective life-long therapy with drugs called tyrosine kinase inhibitors (TKIs). Their response to this treatment is also monitored with a molecular test developed at Imperial in the 1990s, originally used to monitor patients after bone marrow transplant. Professor Apperley explained that researchers realised that when patients relapsed with CML after transplant, they needed to receive treatment quickly to get an effective response, so Imperial researchers worked on finding a way to identify relapse at an earlier stage. This led to Professor Nick Cross, now at the University of Southampton, using polymerase chain reaction (PCR) technology to detect relapses at the molecular stage - before they showed up in the patient’s blood count - allowing for faster and more effective treatment. The test has since been refined to provide a robust and accurate understanding of the level of residual disease. It is now routinely used in developed and developing countries to diagnose, assess response, determine management and predict outcomes for the cancer.
If you respond to tyrosine kinase inhibitors (TKIs), you will never go into blast crisis. And if you don't go into blast crisis, you'll never die of your disease.
“On average, the time for an individual patient to go into blast crisis used to be five years, so the median survival of CML, pre-TKIs, was five years unless you could have a bone marrow transplant,” Professor Apperley said. “After the TKIs, the vast majority of patients have the same life expectancy that they would have had if they'd never had CML.” This change has turned CML into a chronic illness, like asthma or diabetes. “If you respond to the TKI, you will never go into blast crisis. And if you don't go into blast crisis, you'll never die of your disease.”


Better screening for bowel cancer
Another major area of research for Imperial in recent years has been in population-based screening and surveillance for bowel cancer. Under the leadership of Professor Wendy Atkin, who passed away in 2018, a randomised controlled trial of approximately 170,000 adults across 14 areas in the UK was developed to determine whether flexible sigmoidoscopy, which examines the lower part of the large bowel, could reduce bowel cancer incidence and mortality. This screening modality can not only detect cancers at an earlier, more treatable stage, but also allows any precursor lesions for bowel cancer to be removed to reduce the risk of cancer developing.
After a 2010 paper on the trial was published in The Lancet, flexible sigmoidoscopy screening was rolled out by the UK National Screening Committee starting in 2013, with £60m of investment from the UK Government. It was estimated that the strategy could prevent 5,000 cancer diagnoses and 3,000 deaths per year.
“We’ve continued to follow the people in the study and currently we have published data up to 17 years after the screening,” Professor Amanda Cross (pictured), who now leads Imperial’s Cancer Screening and Prevention Research Group, said. “After 17 years of follow-up, the bowel cancer risk among the people who were screened is still significantly lower than those who were not screened."
This chart shows that patients who were screened using a flexible sigmoidoscopy recorded lower incidences of bowel cancer than those who were not screened as part of the trial.
Professor Cross has also worked on the UK’s post-polypectomy surveillance guidelines, which led to a change in guidelines in 2020 to minimise unnecessary invasive colonoscopy procedures. Her research found that among patients recommended three-year follow-up surveillance colonoscopy, according to the guidelines in place at the time, there were two subgroups - with only one of these subgroups being at significantly increased risk for bowel cancer.
This higher risk subgroup included those who did not have a complete colonoscopy, those with poor bowel preparation, those who had polyps (small growths on the inner lining of the colon or rectum) with severely abnormal cells, and those who had large polyps or polyps in the upper part of the bowel. These findings made a vital contribution to the 2020 post-polypectomy guidelines, which could reduce colonoscopic surveillance workload by up to 80%, saving significant money for the NHS and reducing unnecessary invasive tests for patients.

Detecting cancer more quickly
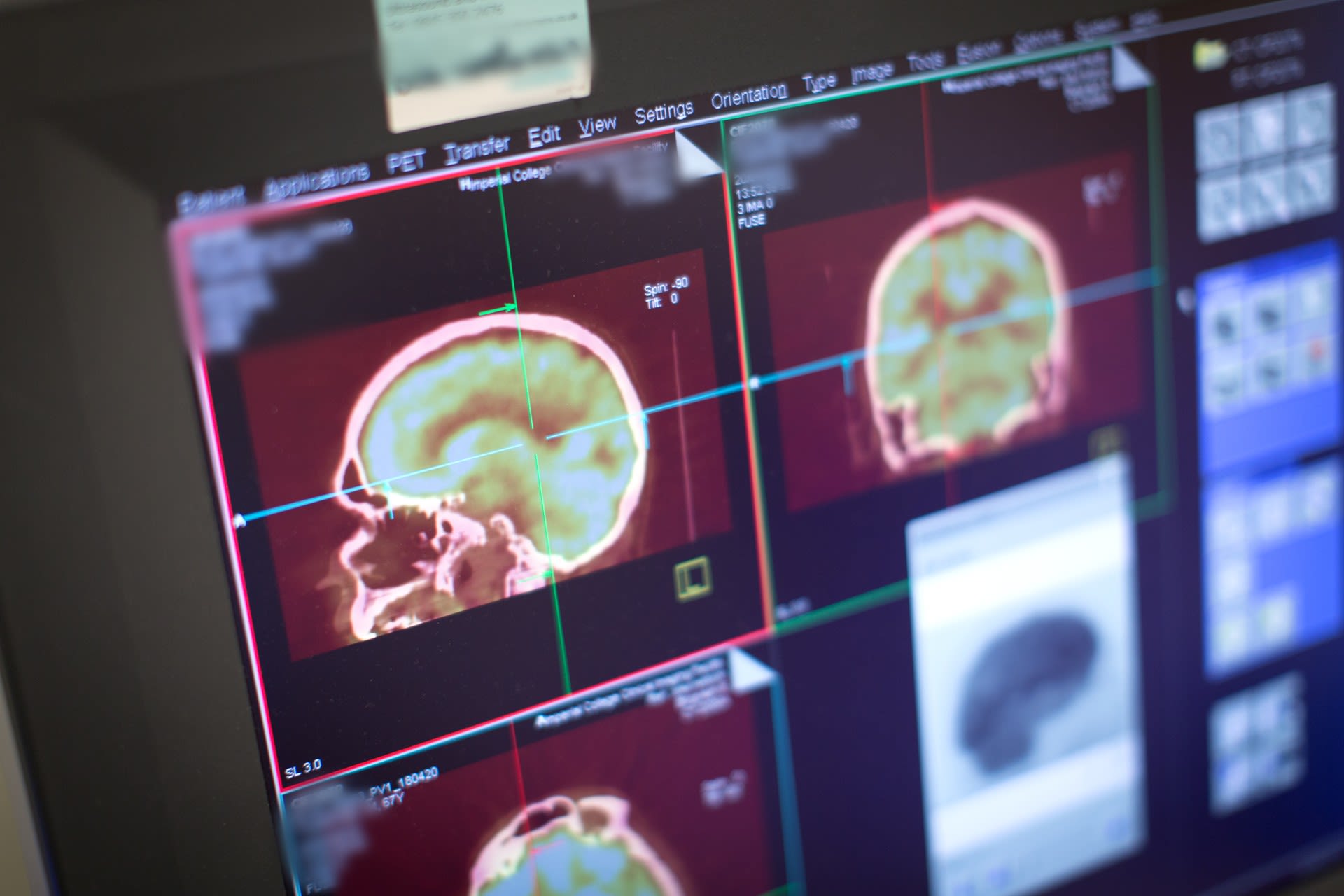
Led by Professor Eric Aboagye, Imperial’s cancer imaging group has worked on improving our ability to detect cancer more quickly and to develop methods that will significantly improve patient care. Through the use of positron emission tomography (PET), magnetic resonance imaging (MRI), and ultrasound (US), researchers hope to cut the time for detecting response to therapy from weeks to days.
Professor Aboagye explains that his group’s work is focused on “visualising the characteristics of cancer in patients” through imaging techniques. In recent years, this has come through anatomical & functional imaging, allowing researchers to see inside the body without the need for surgery.
One of the team’s key success stories is the development of an imaging probe to highlight programmed cell death – a process where a cell dies due to specific transmission of signals inside the cell. Imperial researchers developed the probe to target specific proteins that could highlight tumours that were programming to die. “We did that so that we can see very early, in hours to days, that a cell is going to die,” Professor Aboagye said. “That's important for monitoring response to therapy, to see if we can predict response to therapy very early on. And then if a patient is not going to respond to therapy, their doctor can alter treatment.”
The cancer imaging group’s current interests are in combining diagnosis and treatment in cancer patients through a field known as ‘theranostics’. This links to the group’s radiomics work, which aims to extract information from medical images, such as a CT scan, using an algorithm in greater detail than experts can normally do. “One of the biggest successes we have had there is in ovarian cancer, where we created an algorithm which was able to predict whether a patient would live beyond five years or die within two years - to simplify the findings,” Professor Aboagye said. “I think that sort of tool is quite powerful.” This information, he added, allowed clinicians greater ability to discuss different treatment options with patients based on the prognosis. Theranostics allows us to merge imaging output more directly to therapy choices and particularly highlights use of molecular radiotherapeutics.

Shaping the future of cancer research

Looking to the future, our researchers are thinking about how to improve Imperial’s research by combining the College’s expertise in engineering, physical sciences, life sciences and medicine.
The Cancer Research UK Convergence Science Centre was established in 2018 between Imperial and The Institute of Cancer Research, to develop innovative ways of addressing challenges that cannot be addressed by traditional methods. The multidisciplinary centre aims to integrate experts from different disciplines to co-create new tools, technologies and methodologies for cancer research.
Professor Iain McNeish explained: “It is everything from AI analysis of mammograms - Professor Lord Ara Darzi's work with Google DeepMind looking at automated analysis of mammogram images - through to novel devices that can help us understand the complexity of cancer ex vivo and working with the photonics experts in the Department of Physics to develop methods for real-time three-dimensional analysis of cancer cells.”
The patients help us frame the clinical questions and the research questions, and it's only by having that interface between patients and science that you really make progress.
This approach to research, Professor McNeish added, plays to Imperial’s strengths as an institution, through its multidisciplinary research expertise and its links to Imperial College Healthcare NHS Trust. “We are the regional cancer centre for North West London, so we have access to patients and patient samples,” he said. “The patients help us frame the clinical questions and the research questions, and it's only by having that interface between patients and science that you really make progress. This is fundamental to what we do.”