New device could accelerate the development of T-cell immunotherapies for cancer
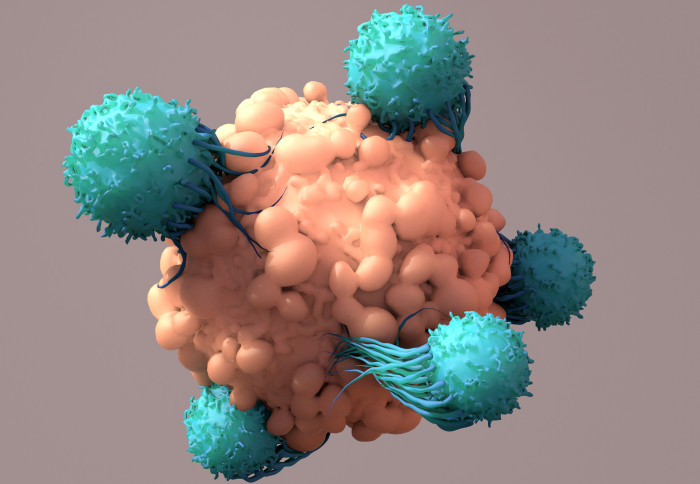
T-cells can be grown and reintroduced to patients to fight cancer
Imperial researchers have invented a device that can rapidly select T-cells that are most effective at attacking cancer cells.
The new microfluidic device, which is being patented in readiness for commercial development, could be used to rapidly accelerate the clinical development of new T-cell based immunotherapies for cancer.
A new approach to cancer treatment
Immunotherapy is an approach to treating diseases that harnesses the body’s natural immune defences. In a relatively new form of immunotherapy known as adoptive cell therapy, immune cells occurring naturally in the human body are isolated and in some cases modified to enhance their ability to kill disease cells such as cancer cells. They are then grown into large populations before re-introduction into patients.
Researchers are aiming to develop new versions of T-cell therapy in addition to other adoptive cell therapies based on a variety of immune cells to treat a wider range of cancers, particularly solid tumours.
Some cellular immunotherapies have already been approved and are being used to successfully treat diseases. CAR-T therapy, which involves engineering T-cells to recognise specific antigens found naturally on cancer cells, entered the market in 2017 and has proved effective at treating blood cancers.
However, adoptive cell therapy is still in its infancy. TCR therapy, a variety of T-cell therapy that is still advancing toward clinical approval, has the potential to be more versatile than CAR-T therapies because the method identifies antigens presented on naturally occurring proteins known as major histocompatibility complex molecules. This allows TCR therapies to target a far wider range of antigens present on the surface of or within tumour cells, stimulating a potent and specific anti-cancer immune response.
Researchers are aiming to develop new versions of both these forms of T-cell therapies in addition to other adoptive cell therapies based on a variety of immune cells to treat a wider range of cancers, particularly solid tumours.
Accelerating development of T-cell therapies
To develop a new T-cell therapy is a lengthy and costly endeavour, costing potentially billions of dollars. Part of the difficulty is the slow process of identifying and isolating effective T-cell clonotypes (set of T-cells with the same receptors) for preclinical research from the trillions of available clonotypes.
It may be possible to dramatically accelerate this stage of research and development using the new microfluidic device designed by Dr Sam Au, lecturer in Imperial’s Department of Bioengineering with PhD graduate Dr Julian Ashby, and evaluated with colleagues at Imperial, the École Polytechnique Fédérale de Lausanne, and Lausanne University Hospital. The team’s microfluidic lab-on-a-chip device is designed to discriminate and recover highly potent T-cells with up to 100% purity from mixed populations of T-cells within 30 minutes.
While existing technologies used to select T-cell clonotypes for preclinical studies examine how well T-cells bind to cancer antigens, the new device is designed to assess a wider suite of interactions between T-cells and cancer cells in a method the inventors call cellular avidity, providing not only a fast result but also a more accurate picture of which T-cells are most effective at killing cancer cells.
The team’s microfluidic lab-on-a-chip device is designed to discriminate and recover highly potent T-cells with up to 100% purity from mixed populations of T-cells within 30 minutes.
In a new publication in Advanced Healthcare Materials, the team say the device is capable of probing 10,000 interactions between immune cells and cancer cells in as little as 30 minutes and could help assess the many co-stimulatory and co-inhibitory signals involved in the activation of T-cells and enable important functional analyses such as to the ability of T-cells to bind and destroy tumour cells.
Lead inventor Dr Sam Au in Imperial’s Department of Bioengineering said: “The method we have developed could dramatically reduce the time and cost of bringing a new adoptive cell therapy to market by rapidly identifying which immune cell candidates are most likely to fail or succeed in clinical trials. We are currently exploring opportunities with industry partners to help refine our method for the eventual benefit of patients.”
Commercialisation opportunities
We value the vital support of our industry partners to commercialise technologies like these and we’re always open to beginning new conversations with prospective partners. Dr Simon Hepworth Director of Enterprise
Dr Simon Hepworth, Director of Enterprise at Imperial, said: “In comparison to current techniques, this device has the potential to accelerate the clinical development of a whole range of innovative immunotherapies.”
“It’s an impressive example of the work Imperial is doing with other organisations around the world to translate insights developed in the lab into advanced therapy medicinal products that could transform patients’ lives. We value the vital support of our industry partners to commercialise technologies like these and we’re always open to beginning new conversations with prospective partners.”
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
David Silverman
Communications Division