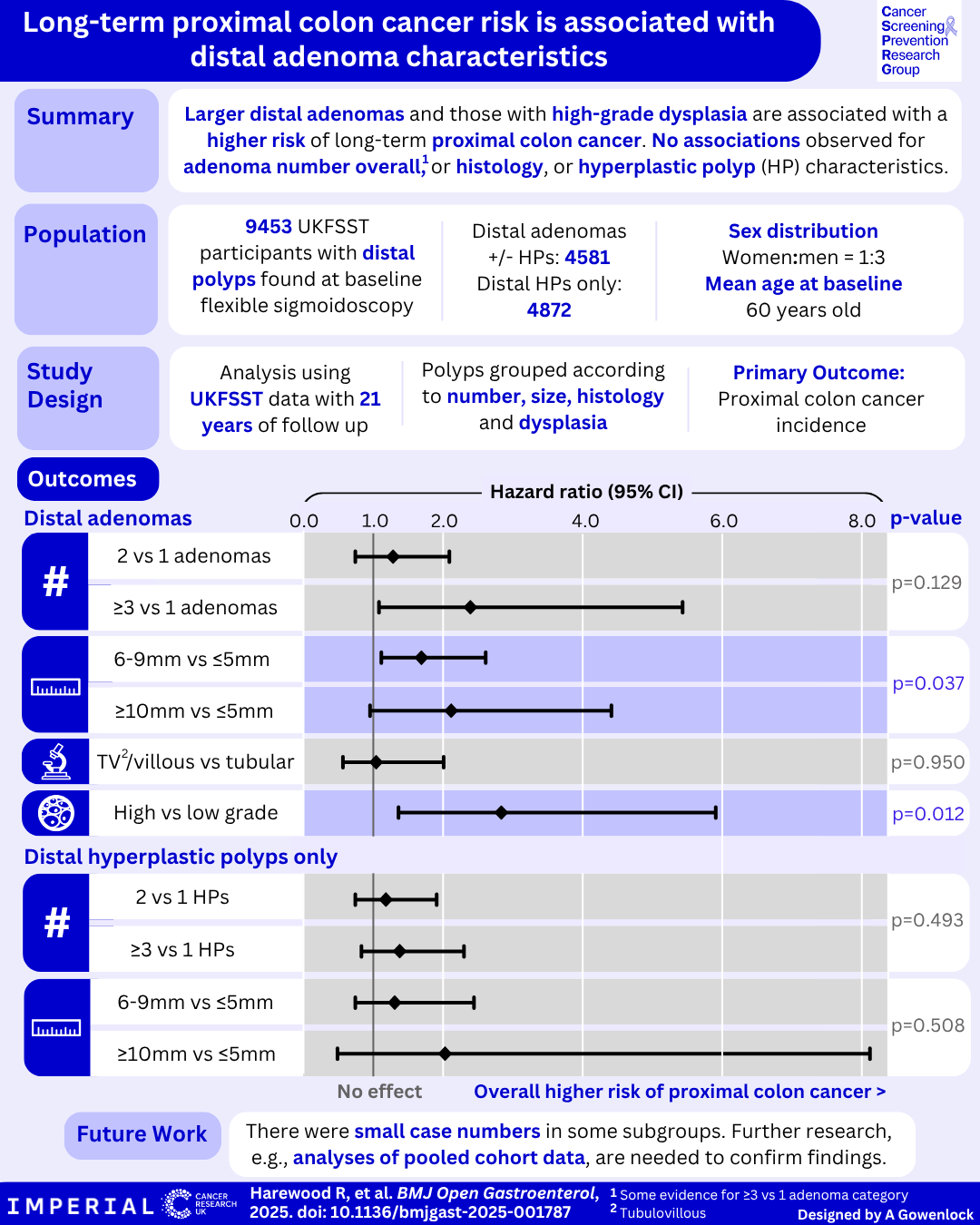
Are distal polyp findings associated with long-term proximal colon cancer risk? New evidence from the UK Flexible Sigmoidoscopy Screening Trial
Our latest paper, published in BMJ Open Gastroenterology, uses data from UKFSST to identify if distal polyp characteristics are associated with future proximal colon cancer risk.
Flexible sigmoidoscopy is an effective colorectal cancer (CRC) screening tool which examines the distal one-third of the colorectum. It can prevent CRC by the identification and removal of precancerous colorectal polyps and is associated with fewer complications and discomfort than colonoscopy, which examines the whole colorectum. The UK Flexible Sigmoidoscopy Screening Trial (UKFSST) previously showed that a single flexible sigmoidoscopy screening exam can reduce CRC incidence by 24% over 21 years. During this trial, despite referral for colonoscopy among participants with ‘high-risk’ findings at flexible sigmoidoscopy, the observed reductions in CRC risk were primarily driven by a reduction in distal CRC but not proximal colon cancer. As around 40% of CRCs arise in the proximal colon, understanding who is at a higher risk of proximal colon cancer is essential.
It is currently unclear whether characteristics of polyps found in the distal colorectum during flexible sigmoidoscopy could help to identify individuals at a higher risk of future proximal colon cancer. This question has major implications for risk stratification and clinical decision making, particularly in determining who might benefit from a colonoscopy and/or colonoscopy surveillance.
Study Design
This analysis included over 9,400 UKFSST participants aged 55-64 years who had distal polyps detected during flexible sigmoidoscopy screening. We examined whether distal polyp characteristics (size, number, histology and grade of dysplasia) were associated with long-term incidence of proximal colon cancer over 21 years of follow up.
Key Findings
Among participants with distal adenomas (+/- hyperplastic polyps (HPs)), larger size (6mm and over) and higher-grade dysplasia were associated with an increased risk of proximal colon cancer.
In contrast, we found no association between the number of adenomas or their histological type and proximal colon cancer.
For those with only HPs, there was no strong evidence that size or number were linked to future proximal colon cancer risk. It’s important to note that sample sizes were small for some exposure subgroups. Further large-scale prospective studies or analyses of pooled flexible sigmoidoscopy trials are needed to confirm these results.
What this means for practice
This is the first study to demonstrate an association between specific distal polyp characteristics and long-term risk of proximal colon cancer. These findings could help clinicians to better identify those at a higher risk of proximal colon cancer and ensure that they have the appropriate colonoscopy screening and/or surveillance. Our findings contribute evidence needed to inform post-polypectomy colonoscopy surveillance guidelines, particularly with respect to size criteria considering the higher risk found for 6-9mm adenomas which are not currently considered high-risk polyps under some protocols.
This study was conducted by Dr Rhea Harewood, Kate Wooldrage, Dr Emma Robbins, Dr James Kinross, Dr Christian Von Wagner, and Professor Amanda J Cross at Imperial College London and UCL. This research was funded by Cancer Research UK and National Institute for Health and Care Research.
Read the full paper here: https://bmjopengastro.bmj.com/content/12/1/e001787