Could serial FIT tests help to reduce the burden of surveillance endoscopy procedures? In our latest BMJ Open Gastroenterology paper, we examine the association between changes in serial FIT values and advanced colorectal neoplasia (ACN) detection rate in a surveillance population.
For some patients with a history of pre-cancerous bowel polyp, regular surveillance by colonoscopy is crucial to protect them against cancer development, but the increased demand for these procedures is placing significant strain on NHS endoscopy services. This new analysis, which used data from our FIT for Follow-Up study, investigates whether serial faecal immunochemical tests (FIT) could offer an alternative approach to colorectal cancer surveillance, potentially reducing reliance on colonoscopies while maintaining patient safety.
The Need for Tailored Surveillance
The development of colorectal cancer can be prevented by the removal of precancerous polyps via colonoscopy. However, some patients who have already undergone polyp removal remain at higher risk of this cancer and require regular surveillance colonoscopies. Unfortunately, the increasing number of surveillance colonoscopies means that they are now estimated to account for a significant proportion of colonoscopies performed in the UK, and this increasing demand is placing a burden on endoscopy services.
FIT testing, a widely available stool-based test that can be easily administered at home, detects trace amounts of blood in stool. FIT testing is already used by the National Bowel Cancer Screening Programme to determine which individuals should be referred for colonoscopy. If FIT could reliably identify the patients at lower risk within the surveillance population, it could enable a more targeted approach where colonoscopies are reserved for those most likely to benefit, and low-risk individuals are protected from the risks of unnecessary procedures.
Study Design
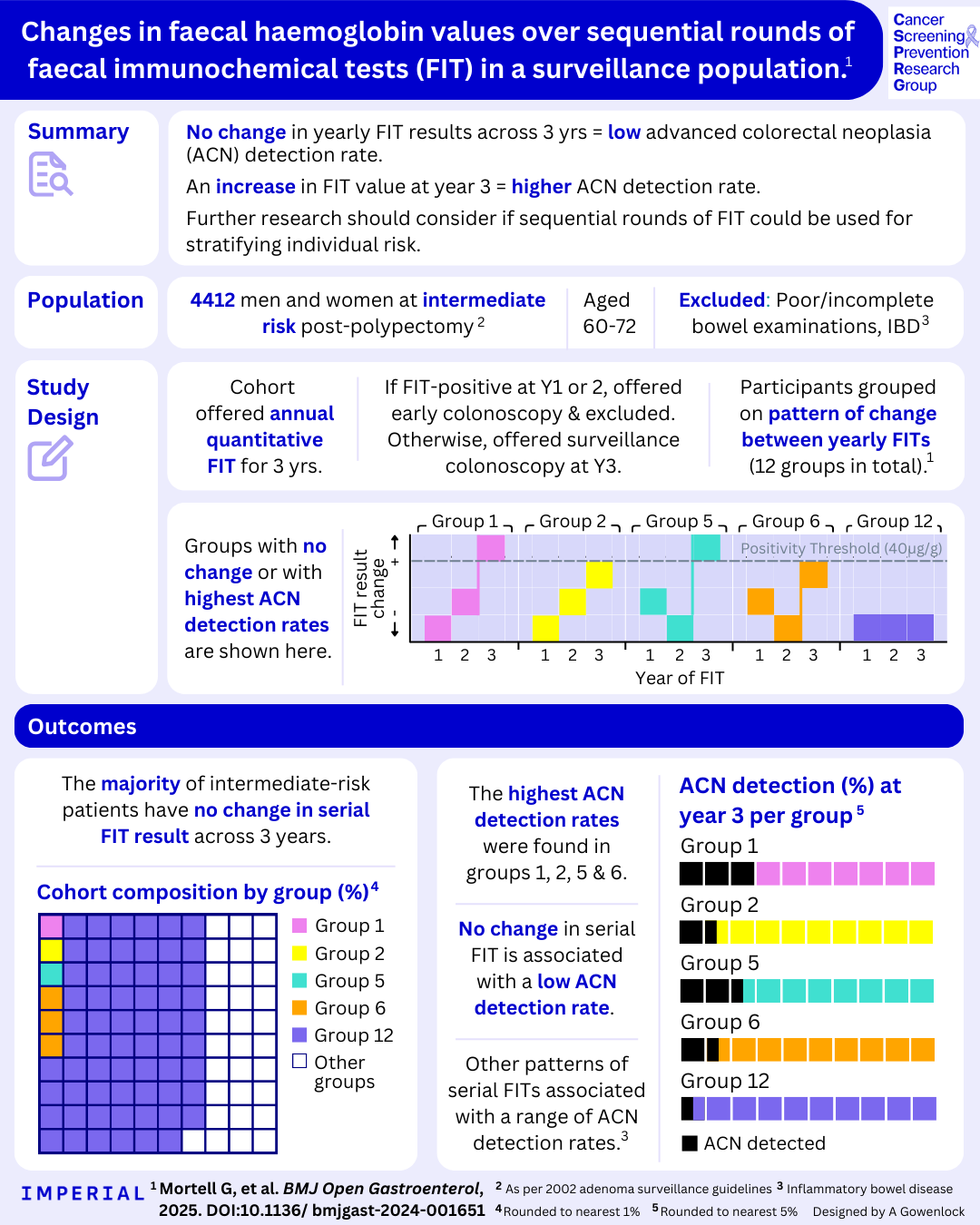
The FIT for Follow-Up study recruited 8,009 individuals aged 60-72 who had previously had polyps removed and were classified as having an intermediate risk of colorectal cancer according to the 2002 UK surveillance guidelines. While these patients waited for their 3-yearly surveillance colonoscopy, they were invited for three annual FIT tests. Those with a positive FIT result at years 1 and 2 were immediately referred for colonoscopy and excluded from the study. The current analysis includes those that had a negative result at years 1 and 2, any result at year 3 and had their year 3 surveillance colonoscopy as planned. This totalled 4,412 participants who were then divided into 12 groups depending on the pattern of change in their FIT results over the three rounds and their positivity status at year 3.
The outcomes measured at colonoscopy were the detection of advanced adenomas or colorectal cancer (jointly termed advanced colorectal neoplasia or ACN). By analysing the trends in the blood found in participants’ stool over three annual rounds of FIT, we aimed to determine whether serial FIT testing could predict which participants were at a lower risk of ACN.
Our Key Findings
We showed that 62.9% of participants had undetectable levels of blood in their stool across all three FIT rounds. Within this group, only 4.7% had ACN detected at their surveillance exam—the lowest detection rate among all study groups.
.png)
The majority of intermediate risk patients have no change in their serial FIT results over three years and have a very low ACN detection rate.
Conversely, the four groups that displayed the highest ACN detection rates all had an increase in FIT value from round 2 to round 3 and all participants in these groups had at least one prior non-zero FIT result. One subgroup of 46 participants with a consistent upward trend in FIT values had the highest ACN detection rate of 32.6% at their surveillance exam.
.png)
The highest ACN detection rates were found in groups 1, 2, 5 and 6. These groups all had an increase in FIT result from round 2 to round 3.
What Could This Mean for Bowel Cancer Surveillance?
Our findings indicate that over half of intermediate-risk participants consistently had undetectable levels of blood found on their FIT tests and very low rates of ACN detected. This suggests colonoscopy surveillance may not be necessary for all intermediate-risk patients, particularly those with consistently undetectable FIT results, raising the possibility of reducing the demand on endoscopy services and protecting those that are least likely to benefit from colonoscopy.
Additionally, the NHS currently reports FIT results as either positive or negative based on a predefined cutoff value. Our work suggests that reviewing absolute numerical FIT values over time could provide deeper insights into individual risk, enabling more informed clinical decision-making.
Looking Ahead: FIT-based Risk Stratification
This trial is one of the first of its kind to assess the role of serial FIT testing in a surveillance population. We provide compelling evidence that multiple rounds of FIT testing could further risk-stratify intermediate-risk patients. Integrating FIT-based surveillance with colonoscopy could enhance colorectal cancer prevention and early detection by freeing up endoscopy resources and ensuring colonoscopies are used efficiently. We hope that our findings will inform future guidelines and contribute to a more efficient, evidence-based approach to monitoring patients at increased risk of colorectal cancer.
This study was conducted by Gemma Mortell, Kate Wooldrage, Dr Gwen Murphy and Professor Amanda J Cross. It was funded by Cancer Research UK.
To learn more about our study, find the paper here: https://doi.org/10.1136/bmjgast-2024-001651