Are We Missing Women at Increased Risk of Proximal Colon Cancer?
Are we missing women at increased risk of bowel cancer? Our newest paper examines bowel cancer risk after flexible sigmoidoscopy.
What is post-polypectomy surveillance?
Bowel cancer develops from bowel polyps. Removal of bowel polyps during an endoscopic examination, such as colonoscopy or flexible sigmoidoscopy, reduces the risk of bowel cancer. Flexible sigmoidoscopies examine the rectum and distal colon (lower part of the large bowel), while colonoscopies examine the rectum, distal colon, and proximal colon (upper part of the large bowel). After polyp removal, some people remain at increased risk of bowel cancer and require an additional colonoscopy (or colonoscopies), typically performed a few years later. This is referred to as ‘post-polypectomy surveillance’.
Why was this analysis needed?
In order to identify which people need post-polypectomy surveillance, studies should compare bowel cancer risk in people not having surveillance with that in the general population. In existing studies, many people had surveillance. This prevented understanding of the true risk of bowel cancer after polyp removal in these studies, as bowel cancer risk would have been affected by removal of polyps at surveillance colonoscopies.
How does our analysis address this issue?
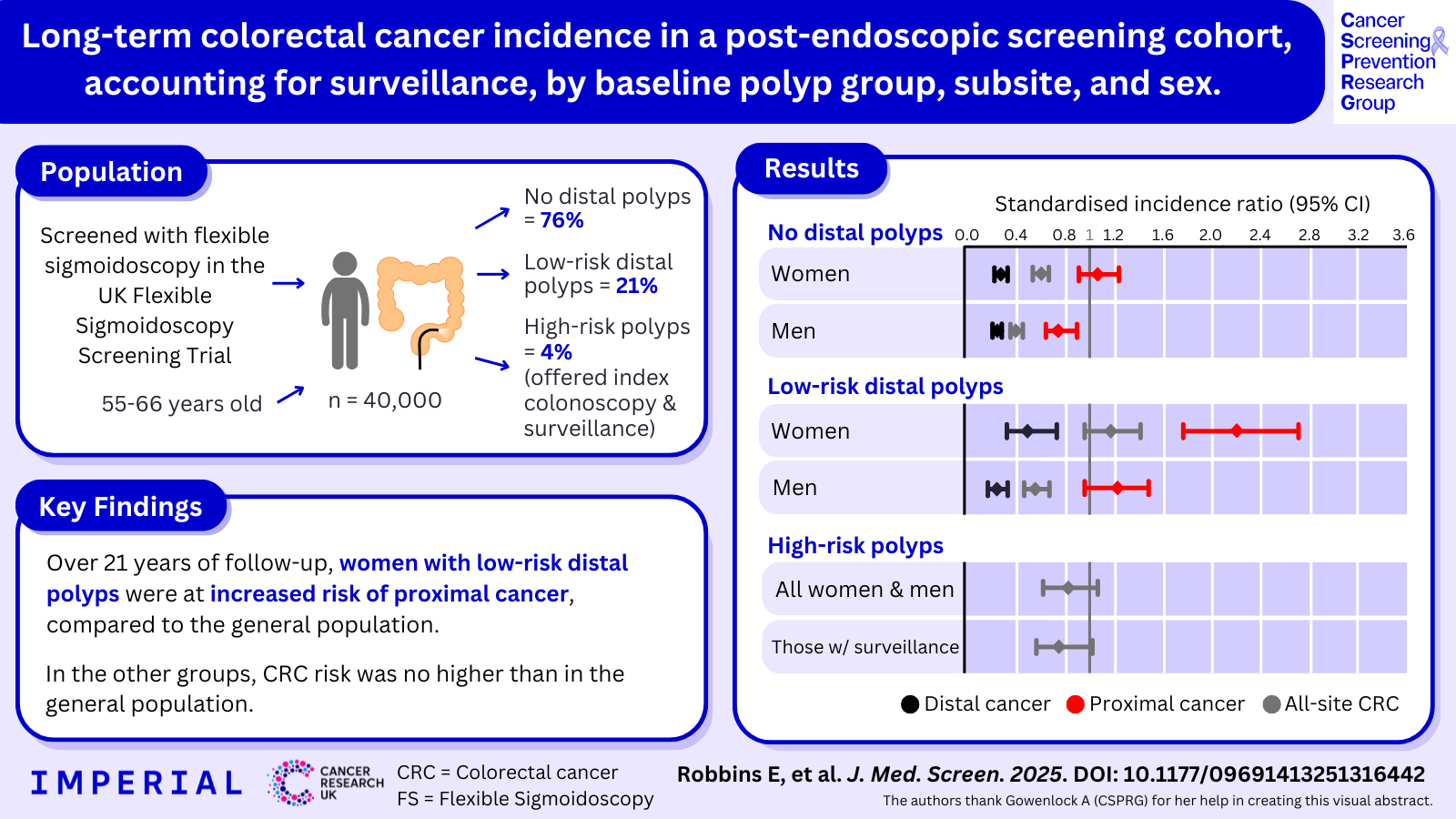
Our latest analysis used data from the UKFSST, the largest randomised controlled trial of flexible sigmoidoscopy screening that has followed over 170,000 participants for more than 20 years. Our analysis included 39,417 UKFSST participants who underwent flexible sigmoidoscopy screening and had:
- No distal polyps - 29,792 people, or 76% of the participants
- Low-risk distal polyps - 8,162 people, or 21% of the participants
- High-risk distal polyps - 1,463 people, or 4% of the participants
All participants with high-risk polyps had a colonoscopy shortly after their flexible sigmoidoscopy (‘baseline colonoscopy’), with 81% undergoing post-polypectomy surveillance, whereas <1% of those with no polyps or low-risk polyps had a baseline or surveillance colonoscopy. That so few participants with no polyps or low-risk polyps had surveillance is unique and enabled us to assess bowel cancer risk after flexible sigmoidoscopy screening, unaffected by surveillance.
What did we find?
Flexible sigmoidoscopy screening, with removal of detected polyps, was sufficient to protect against bowel cancer development over the 21-year follow-up period for women and men who had no distal polyps and for men who had low-risk distal polyps. However, women who had low-risk distal polyps were at double the risk of proximal bowel cancer, compared to the general population, and may have benefitted from having a colonoscopy to protect against cancer development in the proximal colon. Among those with high-risk polyps (who had colonoscopy and most of whom had surveillance), bowel cancer risk was not significantly different to that in the general population.
Implications for the future
These unique data on long-term bowel cancer risk after flexible sigmoidoscopy screening, accounting for the effects of surveillance, may be useful to inform future updates to post-polypectomy surveillance guidelines. We hope that this analysis, and future studies, will help to ensure that people at increased risk of bowel cancer receive colonoscopies, while avoiding unnecessary invasive procedures in people at low risk.
This study was conducted by Dr Emma Robbins, Kate Wooldrage and Professor Amanda J Cross. It was funded by Cancer Research UK.
Read more here: https://journals.sagepub.com/doi/10.1177/09691413251316442