Enzyme with ‘double agent’ role offers new insights into the pathology of asthma
by Ellyw Evans
A novel mediator that drives pathological changes in the airways could be used to spot severe asthma, according to new research.
The findings, published in the journal Science Translational Medicine, shed light on an entirely new mechanism for driving structural changes in airways – also known as pathological airway remodelling – involving a small molecule called PGP. The study demonstrated that PGP was elevated in the airways of patients with the most severe forms of asthma, potentially hinting at a future clinical biomarker and therapeutic target.
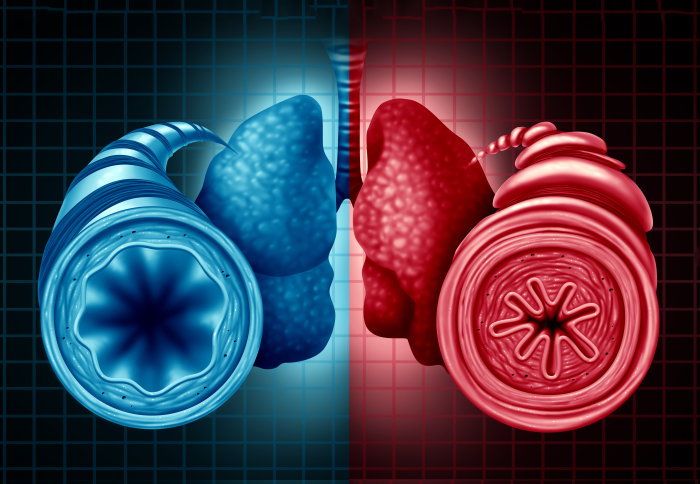
Tissue inflammation and airway remodelling are cardinal features of asthma – a condition affecting 5.4 million people in the UK. It has traditionally been hypothesised that chronic inflammation is driving the airway remodelling and difficulties in breathing that are a symptom of asthmatics.
For several decades, the leukotriene pathways have been implicated as playing a central role in the pathophysiology of asthma. For this reason, pharmaceutical companies have developed drugs that seek to reduce LTB4 and ameliorate inflammation, however, most have failed to demonstrate expected efficacy when tested in patients.
An international team, led by researchers at Imperial’s National Heart and Lung Institute (NHLI), set out to build on their previous research on the role of LTA4H, in which they discovered its unusual ‘double agent’ role in inflammation. Previously LTA4H was thought to solely play a pro-inflammatory role by generating LTB4, however, the team found that the enzyme is unusual in possessing both pro and anti-inflammatory activities.
"PGP may represent a novel biomarker for patients with severe asthma and potentially a therapeutic target to ameliorate epithelial pathology" Dr Dhiren Patel
Specifically, the authors demonstrated in their previous study that LTA4H had an anti-inflammatory role in degrading PGP – a pro-inflammatory signal classically described to cause the recruitment of neutrophils into the lungs. PGP is liberated during inflammation from the extracellular support system of the lung that maintains its architecture and acts as a scaffold for cells, also known as the lung extracellular matrix.
The current study investigated the role of LTA4H in driving pathology in a mouse model of asthma, where mice respond to house dust mite in a comparable way to that seen in asthmatics. The authors found that mice lacking LTA4H and unable to generate pro-inflammatory LTB4 actually found it harder to breathe. This was surprising as these mice experienced less inflammation and therefore should be in better health.
The team revealed that these mice found it harder to breathe as a consequence of PGP accumulation, and a novel neutrophil-independent ability of PGP to act on epithelial cells – the cells that line the airways of the lung – and drive their proliferation and release of sticky mucus. This resulted in narrowing and a ‘clogging up’ of the airways that compromised the ability of the mice to breathe, such as the symptoms asthmatics experience.
Dr Dhiren Patel, postdoctoral researcher from Imperial’s NHLI and author of the study, said: “The findings that we demonstrated in mice are promising in the context of asthma as such changes in the epithelium are seen in patients with severe asthma and we have demonstrated that PGP is elevated specifically in the airways of these patients. Therefore PGP may represent a novel biomarker for patients with severe asthma, and potentially a therapeutic target to ameliorate epithelial pathology in these patients.”
Over recent years, there have been a number of LTA4H inhibitors entering clinical trials for testing in patients with asthma and other chronic diseases, with limited success. The findings of this study may suggest that LTA4H inhibitors in fact inadvertently cause PGP accumulation that could in turn mask any beneficial effects of reducing LTB4.
Dr Robert Snelgrove, Reader in Respiratory Translational Science at NHLI and lead author of the study, said: “Whilst the findings of the study are exciting, they still need to be viewed with caution as much of the work is done in mice and needs to be translated to patients with asthma. It is interesting that we have shown that PGP is elevated in patients with severe asthma, but this needs to be validated in further cohorts of patients and correlated with pathological changes in their airway epithelium and loss of lung function.”
The research was supported by Asthma UK and the Wellcome Trust.
-
“An extracellular matrix fragment drives epithelial remodeling and airway hyperresponsiveness” by Dhiren Patel et al. is published in the journal Science Translational Medicine.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ellyw Evans
Faculty of Medicine Centre