How does convergence science benefit/improve the surgical treatment of cancer?

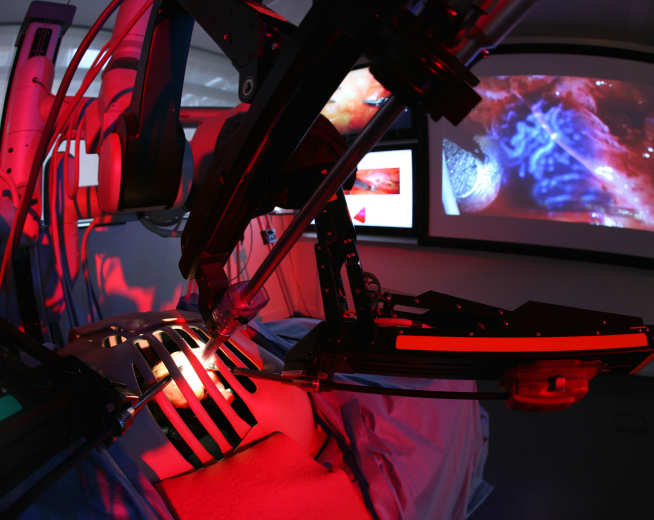
The da Vinci Surgical System represents the successful convergence of medicine and robotics.
This June, CRUK Imperial Centre is hosting a one-day multidisciplinary symposium on Convergence Science in Surgical Oncology.
The event will highlight the importance of convergence science in the development of novel technologies to help improve pre-, intra- and post-operative decision making in cancer surgery.
The symposium presents an exciting programme of world-leading convergence scientists, clinicians and surgeons who will speak across four themed sessions. Session one, on Quality of Life and Survivorship, will be chaired by Mr Daniel Leff, Reader in Breast Surgery, Department of Surgery & Cancer, Imperial College London and will include Prof Jane Maher, Honorary Consultant Clinical Oncologist Mount Vernon Cancer Centre and Clinical advisor Macmillan Cancer Support.
To whet your appetite for the event, we hosted a discussion between the two on the importance of convergence in surgical oncology.
Q: What are the benefits of scientific convergence in surgical oncology?
Mr Daniel Leff (DL): Clinicians whilst being excellent at identifying challenges and roadblocks in cancer care, commonly do not have the technical background or expertise to develop innovative solutions when working in isolation. Given the increasing complexity in our understanding of cancer, it is hugely beneficial to converge multiple science disciplines on to the clinical challenge to expedite the development of technological solutions.
More than this, the integration of a trans-disciplinary language and knowledge transfer means that the future healthcare workforce will be far better equipped to tackle and overcome future challenges in surgical oncology, so that improvements can have real impact on patient outcomes.

Prof Jane Maher (JM): Cancer is changing - it is no longer the binary situation of cure and perfectly normal versus incurable and die quickly. Those who are cured of cancer may have significant treatment related consequences, which requires recognition and management. Whilst those with an incurable disease may live with it for years, with multiple lines of treatments and medicines. Therefore, increasingly we need to be focusing on adding life to years as well as years to life - something that is supported by scientists and researchers converging from across disciplines.
Q: Are the different areas of research naturally converging?
DL: Historically, this has not been the case. Rather, there has been a tendency for clinical, science and research teams to work in silos, hence the protracted timeframe for developments in surgical oncology. Key challenges include the disparate language used by clinicians and engineers, different patterns of working and geographic proximity, all of which have be overcome to realise convergence.
Q: Do we need facilitate convergence? And if so, how?

DL: Yes, at Imperial, key developments in our history such as the merger of medical school with Imperial College and the establishment of the Academic Health Science Centre and Cancer Research UK Centre have enabled collaborations between scientists, engineers and clinicians, with many examples of great success. However, much more needs to be done.
Centres with unique strengths in specific scientific disciplines should be encouraged to work together. I also believe that research training in convergence science should begin at the earliest possible time, so that the common language is embedded within future medical graduates. Finally, there should be greater investment in funding calls with a convergence science theme, and greater opportunities for co-location of science and clinical care so that innovations can be more easily translated to the patients.
JM: Primary Care physicians are generalists with important perspectives on both comorbidities and social context of their patients. There are fewer and fewer opportunities for primary care and secondary care specialists to meet, which reduces opportunities for both effective decision making on prehabilitation or rehabilitation for those with cancer. Creating opportunities for convergence, where hospital-based clinicians and primary care physicians can meet and discuss issues, could pay big dividends e.g. improving relationships, reducing communication problems and creating better patient pathways.
Q: How is your research and convergence science supporting surgical oncology?
DL: As a breast cancer surgeon one of the greatest challenges faced by myself and my surgical colleagues is the inability to guarantee successful cancer excision at the first operation in women who elect for wide local excision (lumpectomy). Nationally, on average approximately 28% of patients need re-operative breast cancer surgery. Myself and my clinical colleagues are working with Imperial scientists and engineers to develop new imaging and sensing technologies that will enable surgeons to better visualise the tumour extent, chemically characterise the tissue at th resection margin and better evaluate the resection bed towards improving the adequacy of the initial surgery, thereby reducing the burden of re-operation rates.
JM: Typically, surgeons have focussed on short term outcomes after treatment rather than looking at quality of life in the months and years later. Our work with Macmillan Cancer Support and others on understanding quality of life may have a significant impact on how choice is offered to patients and the role surgeons can have in pointing their patients towards the resources which will make a difference to outcome.
Q: What do you hope convergence in surgical oncology can lead to?
DL: I have been incredibly fortunate in my career to date, to have had opportunities to work alongside experts in engineering and physical science, and to have witnessed the benefits of these collaborations on the impact and reach of our research. I hope that as examples of success of convergence science become the norm, and not the exception in surgical oncology, we as clinicians will witness a wave of new technologies that enhance the precision of the surgeries we conduct. I hope this will not only maximising the chances of cancer cure but also minimising the risks of collateral damage to normal tissues, helping cancer patients who live with consequences of our interventions enjoy a far improved quality of life in survivorship.
JM: These days, people with cancer will often have more than one illness and see several different teams. Increasingly specialists know more and more about less and less and become less able to judge the relative priority of managing each illness in contributing to the length and quality of life of their patients. This is particularly the case for older patients where effective geriatric assessment and links with geriatric teams can significantly improve outcomes. Convergence in the field, could help these specialists work closer together to help solve all a patient’s issues related to their cancer.
The CRUK Convergence Science in Surgical Oncology Symposium is aimed at a multidisciplinary audience, including surgeons, biologists, physicists, data scientists and engineers. Book your tickets here.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Benjie Coleman
Department of Surgery & Cancer