First findings published from largest home COVID-19 testing programme
A major programme of community coronavirus testing that is tracking levels of infection in England has published its first report.
Tests on more than 120,000 people carried out between 1 May and 1 June, prior to the easing of lockdown, reveal that infection rates were significantly falling, dropping by half every 8 to 9 days.
Led by Imperial College London, the research found that during this period, on average around 1 in 1,000 people tested positive for the virus that causes COVID-19. Rates were found to be highest in care home workers, with 7 positive cases in 1,000. The researchers were also able to estimate the reproduction number (R) – the number of people that an infected individual will pass the virus onto – as 0.57, which is lower than previously reported.
"We’re gathering the critical knowledge base necessary to underpin community testing and facilitate a greater understanding of the prevalence of COVID-19 in every corner of England." Prof Paul Elliott REACT programme director, Imperial
These findings from the REal-time Assessment of Community Transmission (REACT 1) programme are available in a pre-print report and are undergoing peer-review.
The REACT programme, the biggest of its kind, is a series of studies that are monitoring how the virus is spreading across the country. Commissioned by the Department of Health and Social Care, it is being carried out in partnership with Imperial College Healthcare NHS Trust and Ipsos MORI.
The research is offering insight into infection rates broken down by geography, age, sex, ethnicity, key worker status and symptoms. This first report provides a baseline for further research as the programme continues over the coming months, which will be critical to understand the effectiveness of public health measures to control the epidemic and to inform ongoing strategies as the situation evolves.
Professor Paul Elliott, Director of the programme at Imperial, said: “Community testing is a vital step in ongoing efforts to mitigate the pandemic, but to be successful this must be based on robust scientific evidence and sound statistics. Through this surveillance programme with DHSC and Ipsos MORI we’re gathering the critical knowledge base necessary to underpin community testing and facilitate a greater understanding of the prevalence of COVID-19 in every corner of England.”
Understanding coronavirus prevalence in the community
This study found care home staff and healthcare workers were more likely to be infected with the coronavirus during lockdown than the general population, at a time when the public was advised to stay at home and avoid all non-essential travel, therefore limiting opportunities for exposure. The odds of testing positive were almost 8 times higher for care workers, 5 times higher for healthcare workers, and almost twice as high for other key workers.
Those of Asian ethnicity were more likely to test positive than those of white ethnicity. The researchers therefore suggest that higher infection rates could have contributed towards the higher death rates observed in this ethnic group.
"This ambitious testing programme carried out by Imperial will help us better understand the spread of the virus to date, predict how it may spread in the future and inform our response to the pandemic." Matt Hancock Health and Social Care Secretary
Anyone who had recent contact with a confirmed COVID-19 case was 24 times more likely to test positive than those with no such contacts, whereas the odds were 5 times greater in those who had been in contact with a suspected case.
Highest rates of infection were found in young adults, aged 18 to 24, while the lowest were observed in those aged 64 and above. There were no significant differences seen between males and females, different ethnic groups, regions and no evidence of geographic clustering was observed.
More than two-thirds (69%) of individuals who tested positive reported that they were symptom-free on the day of the test or the previous seven days. However, they may have developed symptoms later on and the study didn’t look at how infectious they might have been at this time. Of those who did report symptoms, a number were strongly associated with a positive test, including nausea and/or vomiting, diarrhoea, blocked nose, loss of smell, loss of taste, headache, chills and severe fatigue.
Health and Social Care Secretary Matt Hancock said: “This ambitious testing programme carried out by Imperial will help us better understand the spread of the virus to date, predict how it may spread in the future and inform our response to the pandemic.
“It shows the impact our national lockdown efforts have had and demonstrates that we lifted restrictions at the right time when infection was low.
“As a country we have made great strides towards beating this virus but we mustn’t take our foot off the pedal and such studies will form an integral piece of the puzzle as we continue to safely get life back to normal.”
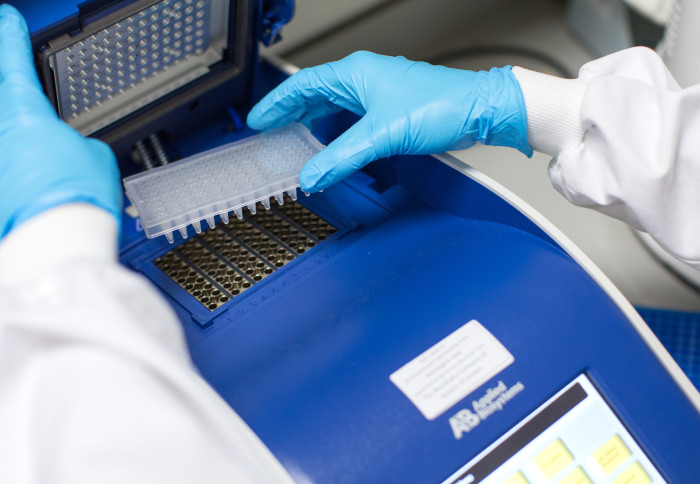
Detecting the virus
To ensure the study sample reflected the general population in England, individuals aged 5 and above from all 315 local authorities were chosen from NHS lists and invited to take part. Invites were balanced according to the demographics of each local authority. Those who volunteered were sent a nose and throat swabbing kit, alongside written instructions and a how-to video. They were also asked to fill out a questionnaire, which gathered information on demographics, living situation and symptoms. The swabs were self-administered but parents or guardians were asked to take swabs of children aged 12 or under.
Participants were asked to keep their samples in the fridge to preserve them and book a courier to pick them up within 24 hours. The samples were then transferred to either Public Health England laboratories or a commercial laboratory for analysis by a technique called PCR, which detects genetic material of the coronavirus.
To make sure that the analyses were comparable between the different laboratories, the researchers carried out a number of different experiments to work out if there were any differences in detection rates and then made adjustments to account for these. This included making a series of dilutions of confirmed positive samples to work out the lowest levels of virus genetic material that the tests were capable of picking up, as well as retesting samples that had given a signal below this level. The researchers then used these findings to set the cut-off point for defining a sample as positive, to minimise the risk of including false positives, where the test wrongly identifies someone as having the virus when they do not in the calculations.
Next steps for the research
This study has been upscaled and repeated for the end of June to the beginning of July, involving over 150,000 participants.
Kelly Beaver, Managing Director - Public Affairs at Ipsos MORI said: “At home community testing at this scale has not been delivered before across England. As a partnership between DHSC, Imperial College London, and Ipsos MORI it has taken significant innovation, perseverance and skill to ensure it has been a success, with lessons learned feeding into future phases of this study and shared with the wider academic community through a transparent publication process. We want to thank all the study participants for their time, and contribution, it has been fantastic to be engaging with the public at this scale on an issue of such national importance.”
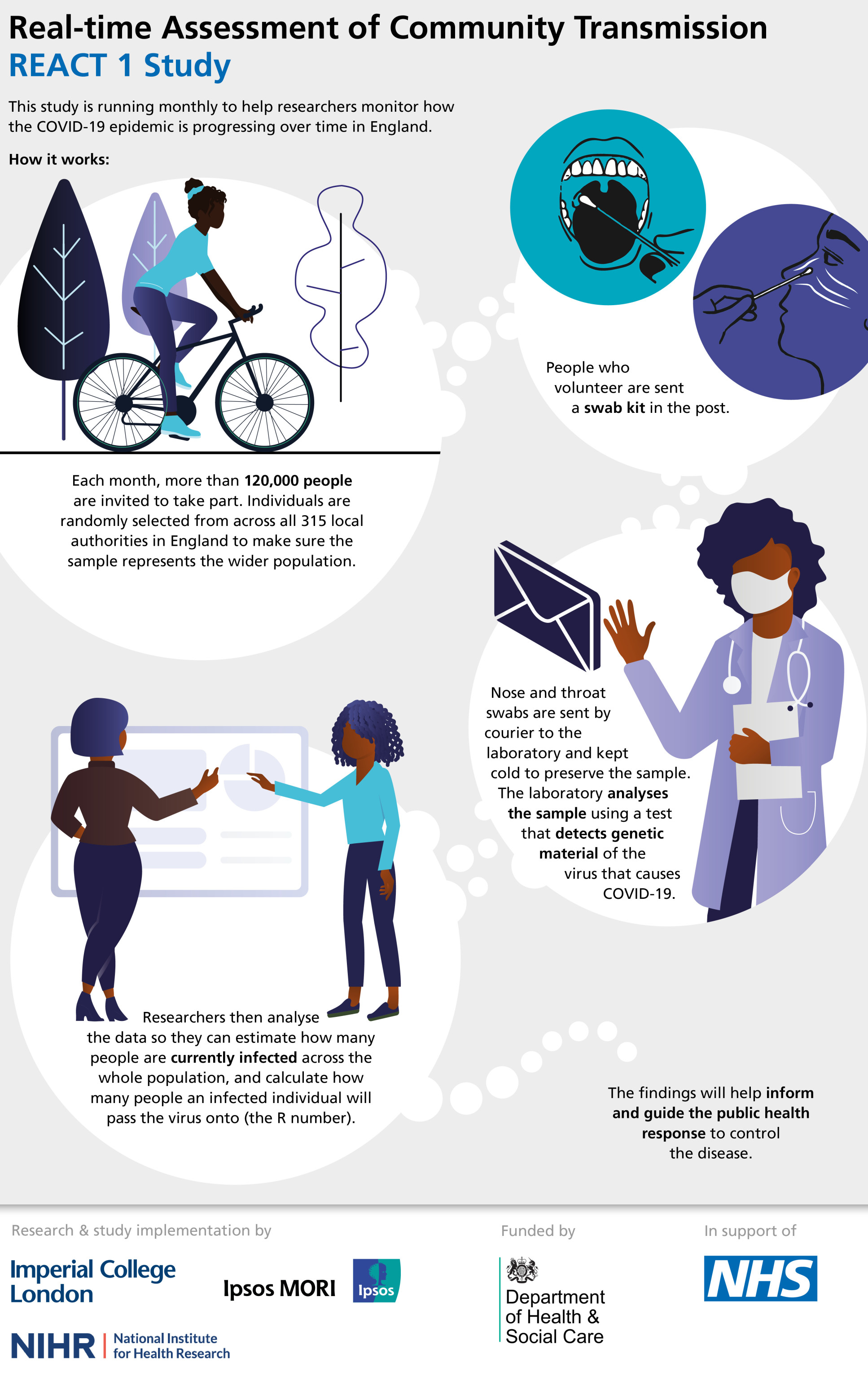
In the second part of the programme (REACT 2), a number of different antibody tests are being assessed for their accuracy and ease of use at home. These tests look for evidence that someone has been infected in the past. This is now being rolled out to over 100,000 people to identify the levels of antibodies against the virus that causes COVID-19 in the general public.
Notes
- Out of 120,610 swab results, 159 were positive. This means the proportion of people who were infected (prevalence) was 0.13%. For care workers, the prevalence was 0.71%, and for health workers 0.47%.
- On 29 May, SAGE estimated R to be between 0.7 and 0.9 in England.
- The pre-print report can be accessed here: https://www.medrxiv.org/content/10.1101/2020.07.10.20150524v1
- Anyone who tested positive or had symptoms of COVID-19, or both, were advised to self-isolate with other members of the household according to Government guidelines. People who test positive are being referred to the NHS Test and Trace for contact tracing.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Justine Alford
Institute of Global Health Innovation