New study explores unique approach to treat a rare liver disease
New research into using a novel approach to alter gut bacteria to treat a rare disease where the body attacks its own liver has been given funding.
The FARGO trial, led by Dr Palak Trivedi of the University of Birmingham and in collaboration with researchers from Imperial, will find out if intervention with a therapy called ‘faecal microbiota transplant’ (FMT) can slow primary sclerosing cholangitis's (PSC) progression and improve quality of life for patients.
PSC is a rare liver disease that affects around 3,600 people in the UK. People can develop the condition at any age, but most commonly those under the age of 40.
In PSC, the body’s immune system attacks the liver, causing inflammation and scarring of the bile ducts. This causes bile to stop flowing properly, and patients experience repeated infections, develop liver failure, and, in some cases, cancer. In four out of five people, the body’s immune system will also attack the bowel, leading to inflammatory bowel disease (IBD) as well as liver disease. The combination of PSC and IBD can lead to around a third of all patients developing bowel cancer and patients require a colonoscopy every year to screen for it.
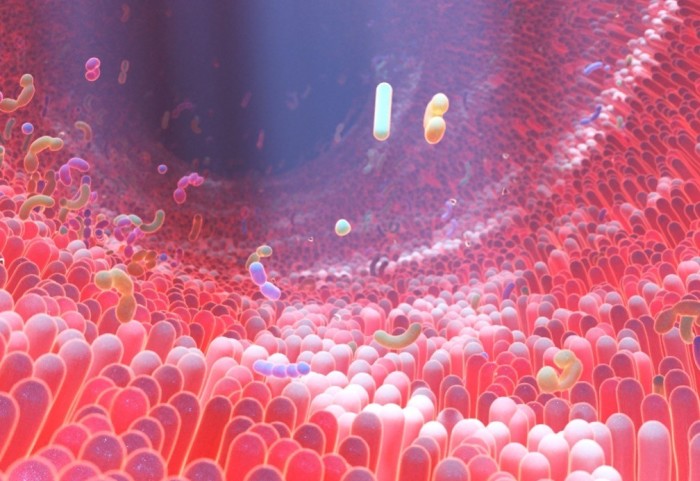
It is known that the microbes present in the gut of people with PSC are different to those in people without liver and bowel inflammation. This gut microbe imbalance is linked with many abnormal immune functions, which may drive the development of the condition.
In the FARGO study, the research team will find out if taking stools containing natural microbes from the gut of healthy donors, refining it in a lab, and transferring it to the bowel of people with PSC, could reverse the imbalance of gut microorganisms. This treatment is called faecal microbiota transplantation, or FMT. Early research has also shown that it may also have a role in treating IBD.
Researchers from the Department of Metabolism, Digestion and Reproduction will work together with those at the University of Birmingham, the Royal Free Trust, and Norfolk and Norwich University Hospitals to carry out a clinical trial to test this new treatment approach. People with PSC taking part in the study will receive either FMT once a week for 8 weeks, or a placebo (an inactive FMT equivalent). Each group will continue to receive their usual routine standard of care for their IBD.
The teams will observe both groups for another 40 weeks. The team will then measure how successful the treatment has been in improving liver blood tests, reducing scarring of the liver, lessening the severity of their IBD, and improving symptoms and quality of life.
Dr Ben Mullish, one of Imperial's team involved in the trial, said: "Our Division has been heavily involved in research into faecal microbiota transplant to help gut and liver diseases for a number of years. As well as supporting clinical aspects of the trial, the Imperial team will also be using the cutting-edge metabolomic techniques of our National Phenome Centre to analyse the bile acids and other chemicals in samples collected from study participants. This will help us to look into mechanisms by which the FMT may be helping patients in a level of detail that has not been done in previous studies".
Dr Palak Trivedi, who is leading the trial at the NIHR Birmingham Biomedical Research Centre said: "This study will really help us to understand which gut microbes are most important, and how this potential treatment could be scaled up to treat more people. Our study will lay the foundation for future work on a larger scale, with a view to making FMT available more globally.
"Should our trial show that FMT works well, PSC Support will be advocating for patients to access FMT as early as possible. We hope this means patients will benefit within five years after we’ve completed this work.”
Currently, doctors treat PSC by managing symptoms only. We don’t fully understand what causes PSC, and there is no cure. A liver transplant is the only life-saving treatment. Although a very rare disease, PSC accounts for 1 in 10 of all liver transplants in the UK and is now the leading reason for liver transplantation in several European countries.
While it is life-saving, liver transplantation is also risky and costly to the NHS. People who have had a transplant must take a cocktail of drugs to prevent their new liver from being rejected. PSC can still return in around a third of people who have had a liver transplant.
The vital funding for this research comes from LifeArc and the patient-led organisation, PSC Support.
LifeArc’s Dr Catriona Crombie said: “Our approach to funding is to work with others, to uncover the potential of promising research that could solve complex healthcare problems that patients face. We’re delighted to be jointly funding this project with PSC Support, which will allow Dr Trivedi’s team to answer key questions and help to translate this experimental treatment, from lab idea towards the clinic, where it could offer hope to patients with PSC.”
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Benjie Coleman
Department of Surgery & Cancer