SPP1: A new drug target to stop the deadly spread of pancreatic cancer
Researchers have identified a new potential drug target to treat & stop the spread of one of the most aggressive & common types of pancreatic cancer.
A team of researchers at the Imperial College London and the Institute of Cancer Research, led by the Scientific Director of the CRUK Convergence Science Centre, Professor Axel Behrens, have identified a new potential drug target to treat and stop the spread of pancreatic ductal adenocarcinoma (PDAC), one of the most aggressive and common types of pancreatic cancer.
Around 10,800 people are diagnosed with pancreatic cancer each year in the UK causing over 9,500 deaths a year. PDAC is one of the leading causes of cancer-related deaths with only 13% of patients surviving 5 or more years1 and 4.3% surviving 10 or more years2.
"Now that we’ve been able to identify key proteins that contribute to its aggressiveness, the next step is to develop a treatment that targets them to hopefully help patients live longer." Professor Axel Behrens Scientific Director of the CRUK Convergence Science Centre
New research published in Nature, shows that there are higher levels of a protein called SPP1 in the blood of patients with later stage pancreatic cancer and this correlates to worse outcomes. When scientists block the formation of this protein in mice, they lived 3 times longer and showed fewer cells that are pivotal in causing the spread of cancer to other organs.
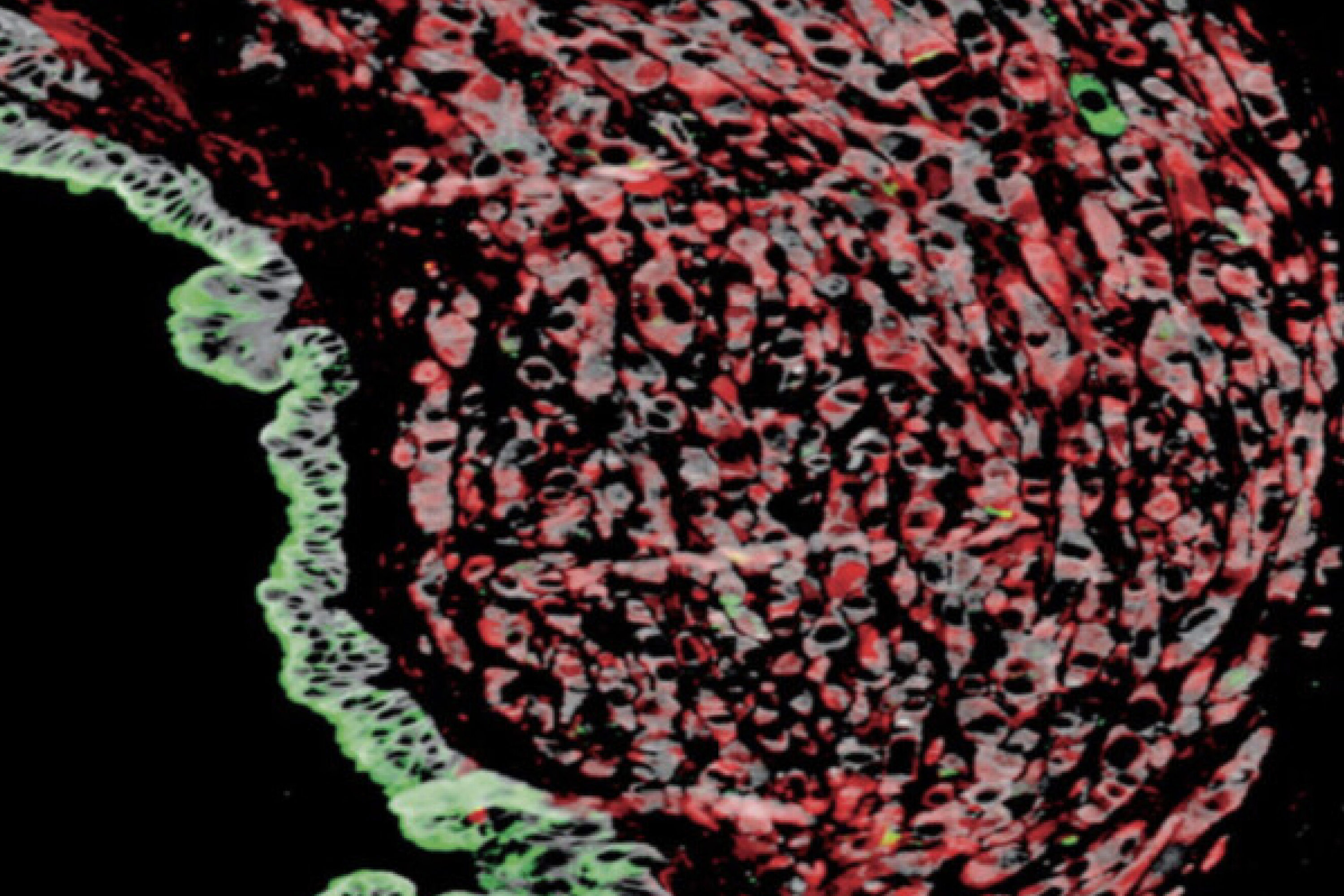
Working with the CRUK Convergence Science Centre's Human Organoid Facility and Biobank, the research team grew pancreatic organoids – a 3D in-vitro cellular model derived from patient samples designed to mimic a tumour environment. When the team switched off the gene that made SPP1, fewer tumours grew compared to when SPP1 was present. Similar findings were also seen in mice with PDAC, where treatment with an antibody to block SPP1 significantly extended their survival with no cancer spread to other organs.
Speaking about the research, Professor Axel Behrens said: “Pancreatic cancer has a long history of poor patient outcomes due to its commonly aggressive nature. Now that we’ve been able to identify key proteins that contribute to its aggressiveness, the next step is to develop a treatment that targets them to hopefully help patients live longer.”
This work builds on previous findings by the same group that found that having low levels of GREM1 protein led to more cancer spread3. This means that SPP1 and GREM1 have directly opposing effects; blocking SPP1 raises the level GREM1 therefore preventing pancreatic cells transforming into more aggressive forms that spread to other parts of the body.
This research paves the way for new treatment to be developed to target SPP1 to treat and prevent the spread of PDAC.
References:
- Li, H., Lan, L., Chen, H. et al. SPP1 is required for maintaining mesenchymal cell fate in pancreatic cancer. Nature (2025). https://doi.org/10.1038/s41586-025-09574-y
- Cancer Research UK – Pancreatic Cancer Statistics
- Lan, L., Evan, T., Li, H. et al. GREM1 is required to maintain cellular heterogeneity in pancreatic cancer. Nature 607, 163–168 (2022). https://doi.org/10.1038/s41586-022-04888-7
Content for this article was adapted from the Cancer Research UK Convergence Science Centre announcement.
Li, H., Lan, L., Chen, H. et al. SPP1 is required for maintaining mesenchymal cell fate in pancreatic cancer. Nature (2025). https://doi.org/10.1038/s41586-025-09574-y
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Article people, mentions and related links
Benjie Coleman
Faculty of Medicine
