Rapid mapping using LQAS reveals impact of treatment in Uganda

Rapid mapping of Schistosoma mansoni prevalence in Uganda, using the Lot Quality Assurance Sampling (LQAS) technique, was carried out over 31 districts during the month of February 2006.
 Rapid mapping of Schistosoma mansoni prevalence in Uganda, using the Lot Quality Assurance Sampling (LQAS) technique, was carried out over 31 districts during the month of February 2006. The survey involved four teams which were made up of three technicians, one of whom acted as the team leader, and one driver. The four teams were assigned different regions of the country (Eastern, Central, Northern and Western) with the aim of sampling 8 schools per day over 3 days per district.
Rapid mapping of Schistosoma mansoni prevalence in Uganda, using the Lot Quality Assurance Sampling (LQAS) technique, was carried out over 31 districts during the month of February 2006. The survey involved four teams which were made up of three technicians, one of whom acted as the team leader, and one driver. The four teams were assigned different regions of the country (Eastern, Central, Northern and Western) with the aim of sampling 8 schools per day over 3 days per district.
The purpose of the rapid mapping exercise was to classify schools according to different prevalence thresholds: <20%, 20-50% and >50%, in order to direct the future treatment strategy for the country programme. The LQAS method is based on the random selection of only 15 children per school and identifying how many of these children are infected or not – with 2 and 7 being the critical numbers. This strategy was based on evidence from a study carried out in Uganda to investigate the validity, applicability and cost-effectiveness of the LQAS method as a rapid mapping tool of S. mansoni (Brooker et al., 2005)
- If all 15 samples are examined and less than 2 samples are positive then the school is defined as a low prevalence (<20 %) school.
- If all 15 samples are examined and less than 7 but 2 or more samples are positive then this school is defined as a moderate prevalence (>=20% and <50%) school.
- If 7 samples are positive then examination can be stopped since this school is already defined as a high prevalence (>=50%) school.
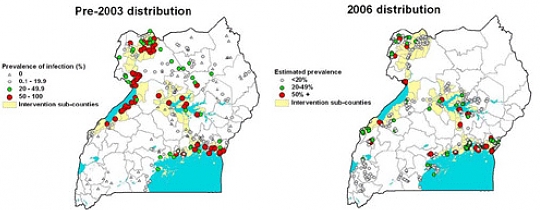
GPS readings for each school were also recorded which allowed, once all the data had been collected, the creation of prevalence maps using GIS software.
 The maps illustrate the impact that treatment has had on the prevalence of Schistosoma mansoni over the country. The most significant effects on prevalence can be seen along the Nile basin in the north-western region of the country and along the shores of Lake Albert. The 2006 map also shows that high prevalence hot spots still exist and it reveals new districts where treatment is required. The 2006 prevalence map will help to direct the future strategy of the Ugandan programme. The plan will be to continue treating schools and communities in the areas where prevalence is >50%.; where prevalence is >20%, and <50% treatment will concentrate on school-aged children only. In the areas where prevalence is below 20% drugs will be provided to the local health facilities for the treatment of any presentable cases.
The maps illustrate the impact that treatment has had on the prevalence of Schistosoma mansoni over the country. The most significant effects on prevalence can be seen along the Nile basin in the north-western region of the country and along the shores of Lake Albert. The 2006 map also shows that high prevalence hot spots still exist and it reveals new districts where treatment is required. The 2006 prevalence map will help to direct the future strategy of the Ugandan programme. The plan will be to continue treating schools and communities in the areas where prevalence is >50%.; where prevalence is >20%, and <50% treatment will concentrate on school-aged children only. In the areas where prevalence is below 20% drugs will be provided to the local health facilities for the treatment of any presentable cases.
 The results of the rapid mapping exercise clearly illustrate that the National Bilharzia and Worm Control programme is achieving its objectives and that with continued support there is a realistic chance of bringing bilharzia infection in Uganda to below an intensity level at which it is a major public health problem.
The results of the rapid mapping exercise clearly illustrate that the National Bilharzia and Worm Control programme is achieving its objectives and that with continued support there is a realistic chance of bringing bilharzia infection in Uganda to below an intensity level at which it is a major public health problem.
References: Brooker S, Kabatereine NB, Myatt M, Stothard JR & Fenwick A. Rapid assessment of Schistosoma mansoni: the validity, applicability and cost-effectiveness of the Lot Quality Assurance Sampling method in Uganda. Tropical Medicine and International Health 2005;10(7):647-658.
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Press Office
Communications and Public Affairs
- Email: press.office@imperial.ac.uk
