PRECISE-DYAD: Health trajectories for moms and their children is led by King's College London with Imperial College London, Aga Khan University, Nairobi, London School of Hygiene and Tropical Medicine, Midlands State University (Zimbabwe), MRC Unit The Gambia at LSHTM, University of Liverpool, St George's University of London and University of British Columbia as collaborating partners on the project. The primary interest of the project is to determine pathways to healthy outcomes for mothers and their children in Sub-Saharan Africa following both normal and complicated pregnancies (Figure 1).
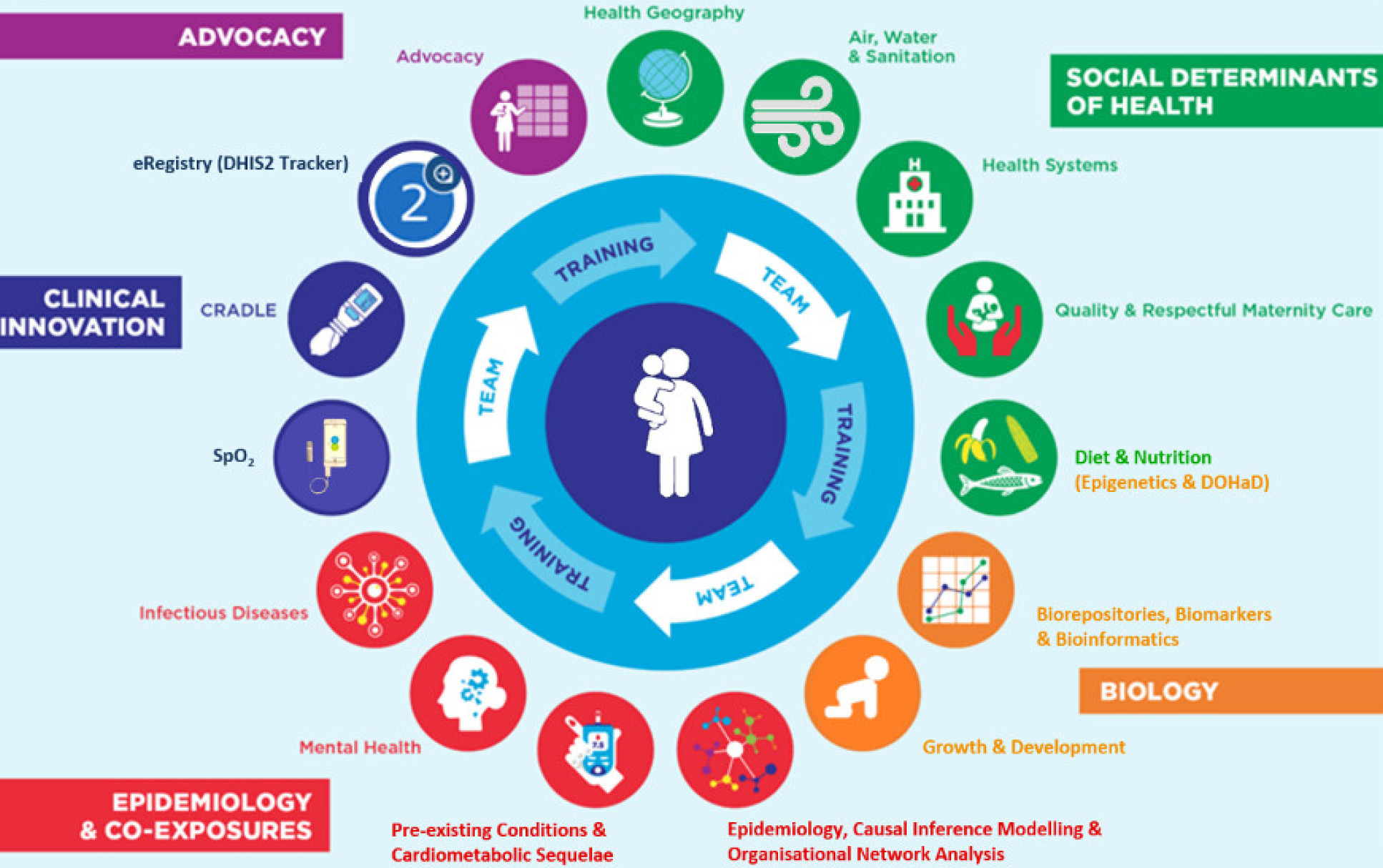
PRECISE-DYAD will expand and extend the PRECISE study (PREgnancy Care Integrating translational Science, Everywhere) of deeply-phenotyped maternal-fetal/new-born dyads to provide insights into the life course of health and disease.
The focus of PRECISE-DYAD is to understand the pathways to healthy longitudinal outcomes following either healthy pregnancies or those complicated by placental complications, namely pregnancy hypertension, fetal growth restriction (FGR), stillbirth, and preterm birth (PTB). The study will follow-up 4,800 mothers and their children in Kenya, and The Gambia over three years.
The PRECISE-DYAD study is jointly funded by The Wellcome Trust and the Department of Health and Social Care (DHSC), through the National Institute for Health Research (NIHR). The PRECISE Study is funded by the UK Research and Innovation Grand Challenges Research Fund GROW Award scheme (grant number: MR/P027938/1).
Air Pollution Exposure and health trajectories within PRECISE-DYAD
There is a looming health crisis in sub-Saharan African countries as they dynamically continue through a protracted epidemiological transition. Much of these transitions have been driven by urbanisation, with its associated multifaceted social, physical and environmental challenges. While African transitions to increasingly urbanised lifestyles present opportunities, these have been exchanged for additional challenges from excessive ambient (outdoor) and household (indoor) air pollution due to dominant use of biomass for cooking combined with high levels of ambient fine particulate matter (PM2.5). The health effects continue to manifest throughout the life course, yet dynamics around causation remains understudied, contributing to double burdens of insufficient evidence and high disease incidences.
Using seasonally-resolved PRECISE and PRECISE-DYAD cohorts of pregnant African women and babies, our component of PRECISE-DYAD will: (i) conduct personal and fixed environmental measurements quantifying dominant sources of ambient and residential air pollution (ii) establish new methods of characterising personal pollution exposures for linkage to health trajectories (iii) investigate contextual patho-aetiologies in pollution/outcomes discourses across contrasting geographies under the assumption of behavioural, geographical, and seasonal dimensions.
Outdoor and indoor exposure measurements will be combined to create personal exposure models indexed to participant geographies. Measurement campaigns will be repeated in the dry and rainy seasons. Measurements will be combined with questionnaire responses and the WHO Global database of household air pollution measurements to extend the sub-sample (PRECISE-DYAD) to the full PRECISE cohort.
The study will utilize the rich PRECISE biobank to explore the micro-geographies of biomarkers and how this may explain the modifying impact of air pollution on maternal outcomes. The study will also complement local surveillance data with satellite derived data for a more granular effect assessment – a lacking avenue in this research domain especially in low resourced settings.
The air quality focus of DYAD seeks to provide a greater epidemiological and mechanistic understanding of health and disease pathways due to environmental stress, in Mozambique, The Gambia and Kenya, following uncomplicated pregnancies and those complicated by pregnancy hypertension, fetal growth restriction (FGR), preterm birth (PTB), and/or stillbirth.
For further information visit PREgnancy Care Integrating translational Science, Everywhere.
PI: Dr Ben Barratt
Social media
Keep up to date by following us on our social channels
Twitter: ERGImperial | YouTube: Environmental Research Group


