Research
Background
Our team is interested in how gene transcription is switched on or off, and how this enables the differentiation and function of insulin-producing cells. This is partly driven by our curiosity, but we also aim to understand disease mechanisms and to develop novel therapies for diabetes.
Mendelian diabetes as a paradigm for disease-modifying therapies
In the late 1990s human genetic studies showed that mutations in transcription factors genes (namely HNF1A, HNF4A, and PDX1) cause Mendelian diabetes. This opened opportunities to understand the molecular underpinnings of specific forms of diabetes. Our work revealed novel regulatory relationships between HNF1A and HNF4A (Boj et al, PNAS, 2001), and identified cell-specific transcriptional programs that are controlled by HNF1A (Parrizas et al, MCB, 2001; Servitja et al, MCB, 2009). We are currently using our knowledge of regulatory networks to develop novel therapies that correct the underlying molecular derangement of HNF1A-deficient diabetes.
Regulatory genomics of pancreatic islets
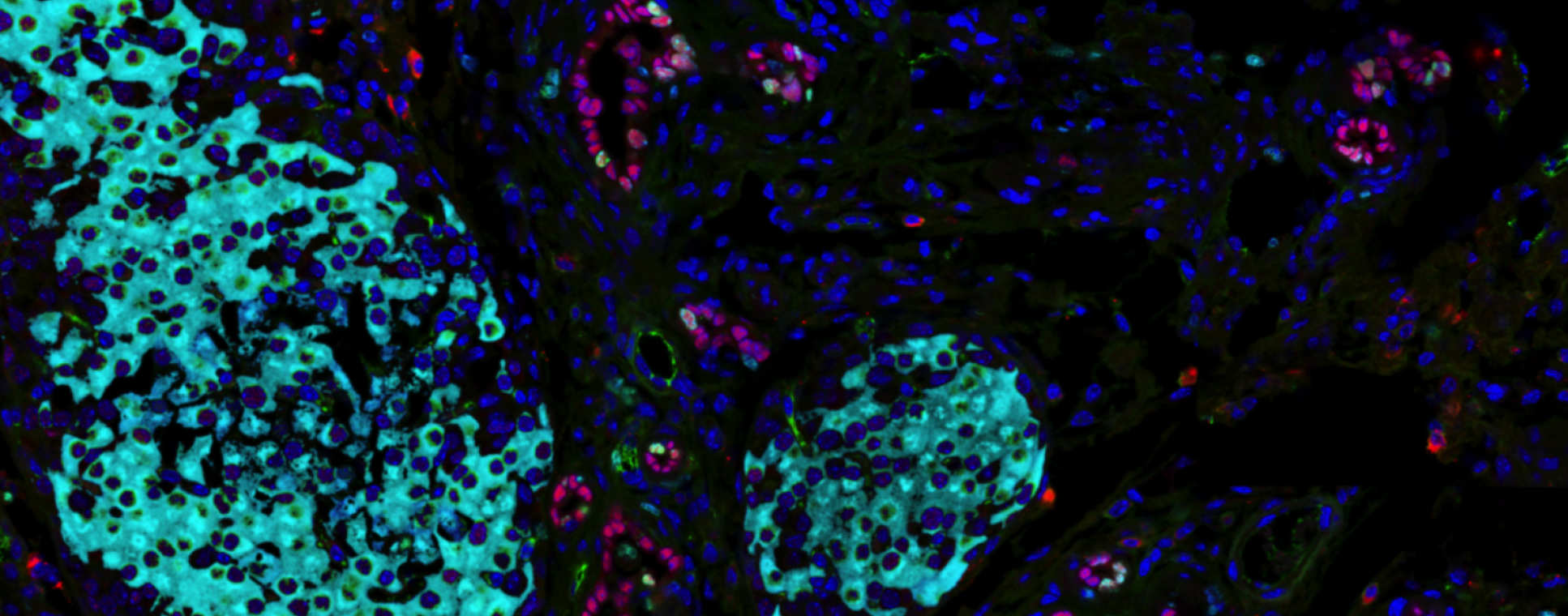
The vast majority of the human genome sequence does not encode for proteins. Epigenomic studies have shown that a large fraction of this non-coding genome space is devoted to regulating gene expression. We are trying to understand how this regulatory information is deployed to create adult functional pancreatic beta cells.
There is accumulating evidence that regulatory genome defects lead to diabetes. We showed that the risk of developing type-2 diabetes is partly dependent on sequence variants that affect the function of pancreatic islet enhancers (Gaulton, Nat Genet, 2010, Pasquali, Nat Genet 2014). Moreover, mutations that disrupt an embryonic pancreas enhancer are the most common cause of pancreas agenesis, a rare form of Mendelian diabetes (Weedon et al, Nat Genet, 2014).
The analysis of genomic regulatory defects underlying human disease is currently in its infancy. It is, however, important to reach an in-depth understanding of disease-causing regulatory defects as this can enable the development of novel therapies. We address this challenge with a broad array of tools, including genome editing in cell-based systems and model organisms, as well as 3D chromatin and transcript profiling in human pancreatic islet samples.
Non-coding transcripts in pancreatic islets
Transcriptome sequencing has recently disclosed tens of thousands of long non-coding RNAs (lncRNAs). We identified thousands of lncRNAs in human pancreatic beta cells, many of which are expressed in a cell type- and stage-specific manner (Moran et al, Cell Metab, 2012). This raises the pressing question of whether lncRNAS might play a significant role in islet biology and disease. We are currently defining the functional impact and mechanism of action of islet lncRNAs.
Regulation of pancreas development and regeneration
Our analysis of Mendelian diabetes and regulatory genomics has led us to identify novel cellular and genetic pathways underlying pancreas development. In one set of studies, we traced the lineage of pancreatic cells expressing HNF1B, a monogenic diabetes gene. The results disproved long lasting views that adult duct cells are a progenitor pool of pancreatic progenitors, and established novel lineage relationships in the developing and adult pancreas (Solar et al, Dev Cell, 2015). In separate studies we defined plastic changes of the epigenome during embryonic development of the pancreas (Van Arensbergen et al, Genome Res 2010, Genes and Dev 2013). We also uncovered a stage-specific combinatorial transcription factor code that controls early embryonic development of the pancreas (Cebola et al, Nat Cell Biol, 2015). Our current studies aim to provide further insight into how pancreatic lineages are programmed, and how genome regulation can be harnessed to promote postnatal pancreatic regeneration.


