Imperial set to lead UK trial of innovative new cancer drug
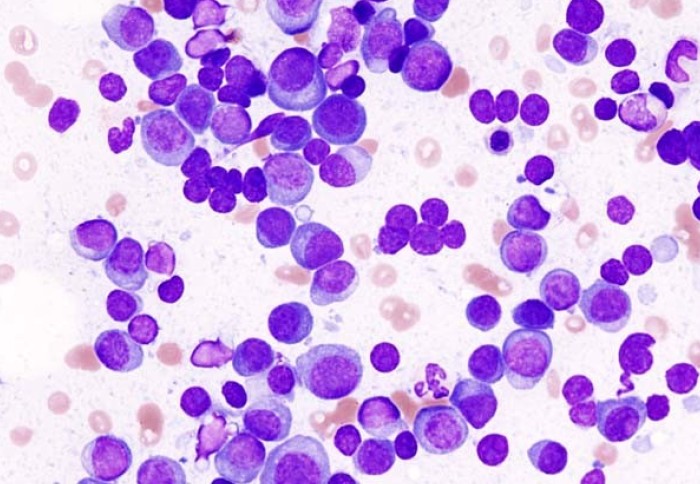
Plasma cells in a multiple myeloma patient
The trial will assess a promising new drug developed by Imperial scientists, designed to treat multiple myeloma and diffuse large b-cell lymphoma.
Multiple myeloma, also known as myeloma, is an aggressive form of blood cancer that develops from plasma cells. Although relatively rare, myeloma incidence grew globally by 126 per cent between 1990 and 2016, with deaths increasing by 94 per cent in the same period. Despite significant progress in research and improved treatment options over the past 20 years, it remains largely incurable.
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma, a type of cancer that develops in the lymphatic system – a network of vessels and glands spread throughout the body. Unfortunately, current therapies only work for some patients with DLBCL, while they are either ineffective or too toxic for many others.
Now, following a £3.7 million award from the Medical Research Council, scientists from Imperial College London are leading a multi-centre clinical trial to assess the safety and efficacy of a new drug developed within the College to treat myeloma and DLBCL.
The study will take place across six UK sites in addition to Imperial: the University of Southampton, the University of Leeds, University College London, the University of Manchester, Cardiff and Vale University Health Board and Nottingham University Hospitals NHS Trust.
Imperial will also work closely with collaborators at the Institute of Cancer Research, the NIHR Imperial Biomedical Research Centre, the Cancer Research UK Imperial Centre and the Hugh and Josseline Langmuir Centre for Myeloma Research.
A novel approach
Previous research has shown that a specific signalling pathway in our cells plays an important role in the development of certain cancers and inflammatory conditions. Normally, the NF-κB pathway helps to regulate our immune system’s response to infection. However, when this goes awry, NF-κB can trigger cells to replicate uncontrollably, causing tumours to develop. This dysregulation also prevents an important process called apoptosis from taking place, whereby cells ‘sense’ abnormality and commit suicide, preventing them from becoming cancerous and spreading around the body.
Over the past 30 years, pharmaceutical companies have unsuccessfully attempted to develop hundreds of drugs to block the NF-κB pathway to treat many different types of cancer and other diseases. One of the main reasons for this failure is that by targeting NF-κB, healthy cells and tissues are impacted as well as cancerous cells, leading to severe unwanted side effects which outweigh any potential benefit to patients.
However, a team of researchers led by Professor Guido Franzoso have developed a new drug which works by blocking the signalling mechanism specifically in cancer cells, leaving normal cells unaffected. By breaking down NF-κB into multiple components, the team was able to identify a cancer-specific survival complex made up of the protein GADD45β and the enzyme MKK7. The new drug compound, called DTP3, works by targeting and disrupting this complex, thereby allowing cancerous cells to commit suicide, with no apparent detrimental effect on healthy cells.
Scaling up and next steps
Previously, a small, early-stage clinical trial involving three patients demonstrated that DTP3 selectively killed myeloma cells in the bone marrow, while leaving the healthy tissue of the patients untouched. Now, the Imperial team will seek to replicate these earlier results and evaluate the safety and efficacy of DTP3 on a larger scale. They also plan to test the effects of the drug on DLBCL, which is currently difficult to treat once it returns following initially successful treatment.
The team will begin formulating the drug for use in the trial in February 2021, with a view to start treating patients in October 2021. During Phase I of the trial, the team will study up to seven different doses of DTP3 in 24 patients to find an optimal dose that is both safe and effective. In Phase II, the study will be expanded to test the recommended dose in two additional cohorts of 24 patients (48 in total) to further evaluate DTP3’s safety and efficacy.
Commenting on the significance of the trial, Lead Investigator Professor Guido Franzoso said: “We have shown that DTP3 works though a new mode of action that gave promising results in the lab and a pilot clinical trial in myeloma patients.”
“We now need a larger trial to establish whether DTP3 is of clinical utility for treating myeloma and/or lymphoma patients. If proven safe and effective in the new trial, DTP3 could be then be used in combination with other drugs to try to improve outcomes in these patients.”
Clinical Chief Investigator Dr Holger Auner added: “It is very exciting to take a drug that was developed at Imperial to our patients, particularly because the safety data from our small pilot study are encouraging.”
Co-Investigator Professor Iain McNeish commented: “We have known for many years that NF-κB is critical in the development of many cancers but specific treatments that target NF-κB have been difficult to develop. That is why DTP3 is so exciting and we are delighted that Imperial College investigators will be leading this research programme”.
Article supporters
Article text (excluding photos or graphics) © Imperial College London.
Photos and graphics subject to third party copyright used with permission or © Imperial College London.
Reporter
Ms Genevieve Timmins
Academic Services