Catching bowel cancer early
A national screening programme to detect the early stages of colorectal cancer – devised by a researcher at Imperial College London – will prevent 3,000 deaths a year once it is fully rolled out.
Related departments and groups
Quick fact
- 43% – the reduction in mortality from colorectal cancer among participants in the UK Flexible Screening Sigmoidoscopy Trial
There are one million new diagnoses of colorectal cancer annually worldwide. It is the third most commonly diagnosed cancer and the second most frequent cause of cancer death in the UK - incurring costs to the NHS in excess of £1 billion annually.
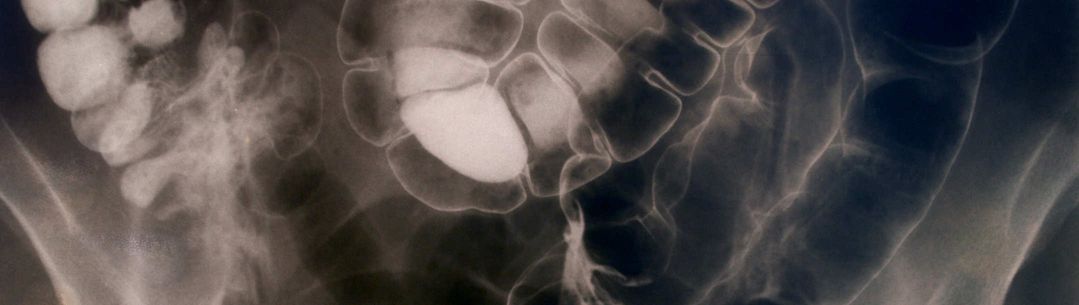
Since 2006 screening for colorectal cancer, also known as bowel cancer, has been offered every two years to those in their sixties and seventies via a home test kit that can detect traces of blood in stools. Suspicious results are then followed up with a colonoscopy examination (a flexible tube with a camera), which looks for the cause of bleeding.
However, this approach misses half of all instances of colorectal polyps (from which colorectal cancer develops) and colorectal cancer itself. This considerably reduces the chances of recovery and survival.
In 1993, Professor Wendy Atkin, now Professor of Gastrointestinal Epidemiology at Imperial, compiled evidence arguing in favour a one-off flexible sigmoidoscopy test, which examines just the lower part of the colon (unlike the more invasive colonoscopy which examines the whole colon), to be carried out at around the age of 60. The idea was that polyps would be detected and removed before the development of colorectal cancer, thereby reducing incidence and mortality rates.
From idea to implementation
Professor Atkin planned the efficient, patient-friendly processes that would be necessary to invite, screen and follow-up the whole population. Those processes are now used in the nationwide programme. She initiated a demonstration project in two areas of London (including a deprived, ethnically diverse region), working with specially trained nurse practitioners to perform the flexible sigmoidoscopy (she also collaborated with the nursing profession in the development of the training programme that is currently in place during its early phase).
In 1993 a small feasibility study involving 4,000 people was performed and a subsequent pilot trial with 16,000 people was undertaken in 1995. Then in 1996 a UK-wide multicentre, randomized controlled trial ‒ the UK Flexible Screening Sigmoidoscopy Trial (UKFSST) ‒ was initiated, involving 170,000 people.
In 2010, the first results of UKFSST were published. The trial showed that 11 years after a single screening, undertaken in men and women between ages 55 and 64, colorectal cancer incidence was reduced by a third and mortality by 43%. The model of delivery was shown to be feasible and cost-effective.
With government backing, the entire screening strategy was rolled out in a national programme from 2013 and is expected to cover the entire population by 2016.
The flexible sigmoidoscopy screening programme continues to be rolled out today. It has been estimated that, with predicted uptake of 70%, flexible sigmoidoscopy screening could prevent 5,000 colorectal cancer diagnoses and 3,000 deaths in the UK each year, and rectal cancer could be rendered a rare disease.
Harpal Kumar, Chief Executive of Cancer Research, UK which co-funded the UKFSST trial, said of the results: "Cancer Research UK does not often use the word 'breakthrough' but this is one of those rare occasions when I am going to. It is extremely rare to see the results of a clinical trial which are quite as compelling as this. Flexi-scope needs to be brought in as soon as possible. Every week of delay will risk scores of lives."


